My story of addiction and recovery is the story of a near miss and an incredibly lucky break. Therapists talk about resilience and protective factors (as opposed to risk factors)—well, I had a boatload of risk factors but somehow I was able to muster some reserves, survive and ultimately thrive.
My story begins when I woke up from a blackout and realized that I had been raped. I remember drinking the night before, but I don’t remember anything from about halfway through the night until the next morning. The other people at the party helped me piece it together—what they saw and heard plus what I felt and what it all added up to. I was 13 years old and was already drinking myself into blackouts. The boy who raped me said he didn’t remember it either. He was only 14.
Within a year I was raped again, this time by an adult—the father of the child for whom I babysat. He was drunk. He was driving me home from babysitting his infant daughter, and made a wrong turn. I knew what was coming and just braced myself for it. I never told anyone.
Stopping One Addiction And Dangerously Starting Several Others
I stopped drinking but I didn’t stop trying to drown. I smoked marijuana, ate Quaaludes, black beauties, and pink footballs; I snorted cocaine, and eventually snorted heroin. I dated a dealer, and did anything I was handed, no questions asked. It came to me one day, an epiphany of sorts: I realized that if I continued to live the way I had been living that I would die. I had stopped short of using needles, but snorting coke and heroin wasn’t getting me high anymore. I had to escalate again, or get clean, or face the reality that life as a heroin addict-garbage head was likely going to kill me.
A mental health professional had said to me that women with my history end up either dead or in prostitution. For a 15-year-old, this was a pretty heavy realization. I wanted to talk with my mom about it, but when I asked her to talk with me later that day, she said no. I pressed her, telling her that I needed her to listen to me. “No,” she said, “I can’t listen to you.”
Pain, Molestation And Addiction At A Young Age
So maybe my story doesn’t begin at age 13 in a blackout after all. If by age 15 my mom couldn’t tolerate listening to me, obviously a whole lot more was going on and had been for some time. I started drinking when I was 12. I wasn’t the only seventh-grader who was drinking, but I was likely the only one who was drinking to deal with flashbacks.
Backing up another year, things had happened that I still struggle to name. Rape is too simple and it conjures up the wrong set of images. Incest is too familial and can’t capture the way it feels when it is your teacher. Yes, my teacher, my sixth-grade teacher.
There aren’t words for what he did; there are sentences. He was a pedophile, and he groomed me for months, setting me up to be in a position where I wouldn’t say no and I wouldn’t tell anyone. He betrayed my trust and he took my childhood at age 11. I loved him and he said he loved me. It was truly confounding. It went on for months, my lies to my mom about where I went after school, my first lies ever to anyone.
It was Lolita, so I’m told—a novel that no matter how wonderfully written it may be, I have never been able to read it. At the end of the school year, he disappeared. Eventually I told a friend, and she told my mom. Police were called, school officials informed. I was interviewed, and then interviewed again by a special police “verifier” to determine whether I was making it all up. I wasn’t.
Choosing Life And Healing In Recovery Over A Life Of Pain And Addiction
After spending the next few years trying to not feel anything, and then choosing to live instead of die, recovery was a very long and difficult road. Not drinking or drugging was relatively easy. Figuring out what to do with all those feelings and how to get my needs met in healthy ways was the real recovery. It took years of therapy, and a passionate will to “be better”—to not only stop trying to kill myself, but to actually enjoy living.
For a while, pursuing some sort of healing was a full-time endeavor. I chased healing and recovery, stalked it, pursued it relentlessly. I was vulnerable to healers of every make and model, and spent money I shouldn’t have spent and time I didn’t have seeking healing.
While I learned a ton and all of it was useful at some level, I think the critical moments were back in my teens when I chose—consciously chose—to live and to live well. I had no idea how I would make that happen, but it was adolescent spunk and contrariness that fueled my strength. Mom won’t listen to me? I’ll show her. In fact, a decent amount of “I’ll show her” propelled me forward through the hardest times. During that critical and vulnerable time, the anger and the desire to show my mom that I would get through this without her help was probably the single biggest protective factor I had going for me.
Reconciliation With Self And Family
Mom and I are reconciled now. We rarely talk about what happened—it is still a sore subject for both of us. Her pain at failing to protect me from a predator is a wound from which she’s had to heal. The rough ride through my teens is something I’ve had to move past—not easy when I was invited to witness teenage years all over again, ringside, as my daughter grew up. Now she is 19 and more whole and healthy than I think I ever have been, and while I can’t take credit, at least I can say with some relief—my past did not infect her.
At some point in my 40s, I stopped chasing down healing. Not that I declared myself finished with that project, but more to the point I realized that no one is ever fully finished. I am back on a level playing field. The challenges that were tossed in my path when I was young no longer haunt me and I am truly happy with my life. I’ve been through a few dark tunnels, and who knows, maybe more will come my way. But for now, for today, I can feel all I feel and deal with whatever comes my way. Life isn’t perfect, but it is good enough.
24 Sep 2013
Do Teens Know the Truth About Molly?
Who is Molly? Molly is the new name for the decades-old drug ecstasy, the drug that was responsible for three deaths and four people being hospitalized in critical condition over this past Labor Day weekend.
Description Of Molly
Molly is a synthetic, or man-made, drug. It first showed up on the streets in the 1980s as ecstasy. At the time it was called a club drug because young people enjoyed taking it when they went dancing, attended concerts or large parties. Today it’s sold in powder form, usually in capsule form but also sold as pills or tablets, with “Molly” connoting molecular purity.
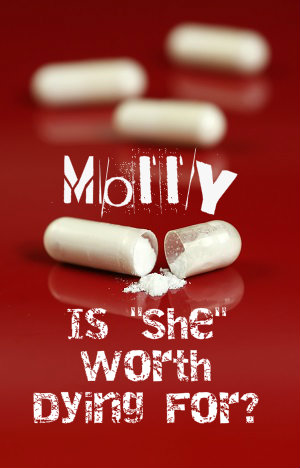 The pills are brightly colored and sometimes emblazoned with cartoonish images. Officially the drug is known as MDMA, which stands for 3,4-Methylenedioxymethamphetamine. If you saw a few words in there you thought you recognized like amphetamine and meth you were right. The drug is a stimulant, or amphetamine, resembling methamphetamine in the way it increases heart rate and stimulation while providing feelings of euphoria.
The pills are brightly colored and sometimes emblazoned with cartoonish images. Officially the drug is known as MDMA, which stands for 3,4-Methylenedioxymethamphetamine. If you saw a few words in there you thought you recognized like amphetamine and meth you were right. The drug is a stimulant, or amphetamine, resembling methamphetamine in the way it increases heart rate and stimulation while providing feelings of euphoria.
MDMA is a concoction combining a stimulant with an empathy-boosting chemical plus a psychedelic. Kids like to take Molly at large group events because the drug makes them feel more energized, less inhibited and closer to those around them. There’s also a sensation of heightened alertness.
Molly’s Risks
There’s also a down-side as it can lead to blurry vision, racing blood pressure and heartbeat and muscle cramps. Sometimes the person’s insides are so revved up that they develop hyperthermia. Long hours of dancing and pressing up against people in a crowd make heat stroke likely. Increased heart rate can easily become an arrhythmia or erratic heartbeat, and seizures have also been known to occur.
MDMA may ratchet up energy and perception but it often pulls down the user’s emotions, leaving them feeling depressed, sad and anxious. Problems with memory can result and these difficulties sometimes last up to a week or more. When a young person decides to mix MDMA with alcohol they increase the sedative effects as well as increasing their risk of becoming dehydrated.
The risk of dehydration with use of MDMA is real, so lots of users try to compensate by drinking more water. However, since it causes the body to retain fluids, the combination of MDMA and water can quickly create an imbalance of electrolytes. Kids who choose to combine Molly with caffeine increase their risk of dehydration while also dangerously increasing body temperature.
Impure MDMA
Called Molly because of supposed molecular purity, the drug is no more pure than any other illicit drug. In fact, MDMA is often cut or completely replaced with another substance known as PMA which produces similar effects. Some deaths attributed to MDMA have actually been caused by PMA. More than that, street drugs are made with no regulating oversight, meaning every batch is unique and users can’t expect one tablet to affect them precisely the same as the last. Many high profile deaths come about because a celebrity is using street drugs in a new city and expecting them to be exactly like those they used in another city — it just doesn’t happen that way.
Celebrity Push Of Molly
Ecstasy, MDMA, Molly — whatever you call it, the drug is enjoying renewed popularity spurred on by pop singers like Madonna, Kanye West and Miley Cyrus. The Monitoring the Future studies conducted by the National Institute on Drug Addiction report that MDMA is experiencing a resurgence among 20-somethings and even high schoolers.
Strong Opportunity For Parents And Teachers
The recent tragic deaths at the Electronic Music Festival in New York provide an opportunity for parents and teachers to talk with teens about the realities of using drugs like MDMA. No matter what pop singers or friends might say, no experience is worth dying for.
11 Sep 2013
Signs That A Teen May Be Using Marijuana
Being a parent carries with it many frustrations, but perhaps none more than suspecting your teenager of regularly smoking marijuana. You wonder, but are not sure. You hesitate to ask directly, but some things just don’t add up.
Here Are 10 Signs That A Teen May Be Using Marijuana:
1. Paraphernalia – If you find joint clips, papers, a bong or pipe in your teen’s room or book bag there is good reason to believe they are using marijuana. These are not the signs of experimentation but of regular use; they definitely do not belong to a friend regardless of what your teen may say.
2. Eye Drops – If you find that your teen is using Visine or other eye drops it’s a pretty good sign they’re smoking dope. If there was a normal problem with your teen’s eyes, most likely he/she would have come to you and spoken about it.
3. Air Fresheners, Incense, Breath Fresheners – If your teen develops a sudden concern over the smell in his room, on his clothes or even his breath it’s worth asking what it is he/she is trying to cover up.

4. Pot Symbols – For some reason, kids who smoke marijuana enjoy advertising their pot use. Posters with pot leaves or stickers/pins with the numbers 420 broadcast to others an above average interest in marijuana.
5. Talking in Code – Most teens are extreme about their privacy, but if you notice that your teen begins using code words when you walk by or regularly leaves the room with his phone when you are around, it could be they are talking about drugs.
6. Finger Burns – If you notice burns on the tips of your teen’s thumb and forefinger it’s probably the result of smoking a joint to the very end. These particular burns are hard to explain in any other way.
7. Isolation or Depression – Again, teens do like to be off on their own, but parents can tell the difference between independence and isolation. If your teen seems depressed and insists on being alone in his/her room rather than taking part in family activities, it deserves investigation.
8. Academic Slippage – A drop in grades is a common sign of drug use. Problems with teachers or school officials and other behavior problems can be a red light signaling deeper issues.
9. Looking for Reasons to Be Out of the House – If your teen suddenly comes up with excuses to leave the house at night you need to find out why. It isn’t likely that your teen suddenly cares about the trash getting out or the dog wanting some exercise.
10. Lack of Motivation – If your teen is no longer interested in things that he/she once enjoyed, or is hard to motivate toward anything, this is a common side effect of pot smoking.
Read More About A Dangerous Drug Trend In Teens
When it comes to teen alcohol and drug use, it seems like there’s always a new method that young people are finding to get high – chugging cough medicine, sniffing glue, snorting bath salts or mixing old medications found in the family medicine cabinet. While it’s normal to be curious, one poor decision can change a person’s life forever.
That’s why authorities and health officials are concerned about a dangerous new trend: smoking alcohol. Because the lungs have such a large surface area, alcohol is absorbed at a much quicker rate when it is inhaled using vaporizers, i.e.: dry ice and bicycle pumps connected to old plastic bottles.
Breathalyzer Comparison
According to Dwayne Baird, spokesperson for the Utah Department of Public Safety, one reason individuals may choose to inhale alcohol is because they believe it won’t show up on a breathalyzer. But Baird says that anyone who understands how the test works knows that a breathalyzer assesses the blood alcohol content and inhaling alcohol actually leads to a higher concentration.
Another reason that people choose to smoke alcohol instead of drink it is that inhaling directly into the lungs delivers a quicker, more intense high. Under normal circumstances, alcohol would be consumed then pass through the body’s stomach and liver where it takes time to metabolize. Dr. Barbara Crouch, Executive Director for Utah Poison Control, equates the practice to binge drinking – when too much alcohol is consumed too quickly, the body has a difficult time successfully processing all of it.
Baird says that the Department of Public Safety still runs across more cases of normal alcohol consumption than it does inhalation methods, but with information able to spread rapidly through social media sites, its popularity with teens could spike quickly.
Scary Results
The body has normal ways of signaling that it has had too much alcohol. When someone drinks to excess, the body responds by causing a person to vomit. That doesn’t happen when alcohol is inhaled. Instead, it passes straight through the lungs into the bloodstream and up to the brain. The problem with that, says Baird, is that it’s difficult for a person to tell when they’ve reached their limit.
Young people in particular tend to regard themselves as invincible and often don’t consider the consequences of their actions or how such consequences might impact their future. But inadvertent alcohol poisoning is a real and even bigger threat when inhaling than drinking alcohol.
Daphne sat across the table from her husband and mouthed the words, “I hate you.” Then she painted a charming smile on her face and ordered a salad. She and Sam were out to dinner with his family, something they did only rarely because of what Sam’s mother referred to as “Daphne’s drinking problem.” What no one at the table knew was that Daphne had a gram of cocaine in her clutch and no plans to drink more than one cocktail. To everyone’s surprise, a single margarita is all she had that night.
For the next four weeks, Daphne’s behavior was erratic. She didn’t find herself sneaking bottles of wine or vodka, passed out on the sofa in front of the television or lying in the floor of their shared walk-in closet, crying her eyes out over every conceivable wrong done to her in the past. Instead, she was scarce, hardly ever at home. When he did see her, she was wild with energy and ideas, frenetic to dress and shower and be off again. Her already thin frame appeared unusually slight. It didn’t look as though Daphne had been eating, or really doing anything but moving, fast.
Then on a Sunday afternoon, just like it had started, Daphne was suddenly home again—collapsed on the lawn, so drunk Sam could nearly smell the alcohol from the front door. Ever the co-dependent faithful partner, he walked to his wife and bent to scoop her into his arms. And just like clockwork, Daphne began to slur a litany of praise for her husband, how she could not live without him, how he was perfect in every way.
Days into Daphne’s return, however, she was threatening to stab herself with a kitchen knife if Sam didn’t give her access to all of her pain medication. Daphne received prescription opiates for a cracked cervical vertebra, and Sam sometimes hid them when Daphne’s drinking binges got especially bad. When she took the knife and started carving shallow cuts into the inside of her arm—something Daphne had done many times before, but always in private—Sam knew it was time to do what he had not yet done. He had his wife involuntarily hospitalized. An emergency hospital stay turned into a longer, voluntary in-patient psychiatric stay, and it was there that Daphne was formally diagnosed.
She was an alcoholic. She was a drug addict. She had anorexia. She had bipolar disorder. And she had borderline personality disorder. No one had expected this outcome, least of all Daphne.
Mental Disorders and Addiction
When a person has both a problem with addiction and a mental disorder, he or she is said to have a dual diagnosis (or comorbidity). Many times, substance abuse can mask the signs of mental illness. Traits or characteristics of mental illness, which may otherwise be quite noticeable to close family members and loved ones, cloak themselves in the depressed behavior brought on by excessive alcohol use (alcohol is itself a depressant), or the erratic behavior others exhibit whether using alcohol excessively or when high or seeking drugs.
People with certain mental disorders may seek to “self-medicate” the anxiety or depression that arises as a result of the disorder by consuming alcohol or using drugs, or a combination. One such disorder is bipolar disorder. About 56 percent of people with bipolar have experienced drug or alcohol addiction. The personality disorders, such as borderline personality disorder (BPD), also share a high rate of dual diagnosis. According to the Center for Drug and Alcohol Programs at the Medical University of South Carolina, “Over 50 percent of drug abusers and almost 40 percent of alcoholics have at least one serious mental illness.”
Besides bipolar and BPD, depression, anxiety disorders, schizophrenia and other personality disorders frequently co-occur with substance abuse. Psychiatric issues can begin before or after the onset of substance abuse.
Treatment for the Dual Diagnosed
There is no question that adding disorders and substance issues to the mix significantly compounds an individual’s stress and further complicates treatment options. Those who have co-occurring mental disorders have a higher rate of relapse when it comes to getting sober. But even people with mental disorders and co-occurring substance abuse issues can begin to heal. What helps is an integrated therapeutic approach—where mental health treatment and addiction recovery are not thought of as separate, but fused into an integrated whole. Compartmentalizing too many areas of her life is often how an addict with mental health issues gets to the place in which she desperately needs recovery, so seeing her life as a working whole is important.
Thinking, “I cannot attend to my sobriety if I do not attend to my bipolar disorder” and vice versa is a good way to think about it. It’s quite true, in fact—not simply a bromide offered by practiced faces in the business of therapy.
While Daphne’s situation may seem extreme, it is likely that the deeper part of her issues are connected. When she begins to do the work to unravel what the deeply held beliefs and long-held stories that most affect her mental state are, she may begin to find herself experiencing better balance—and an ability to deal with the boat-rocking experience of finding herself with a half-dozen labels, all too frightening to think about in the beginning.
Becoming educated about the nature of addiction and the reality of mental illness is a good place to start. Choosing to look at one’s life carefully is the opposite of what addiction means. When you wrestle the hydra of addiction and mental illness, you know you’re only going to get more of the same. Better not to go in swinging but with clarity, a willingness to learn and possibly, maybe, a little bit of room for something like hope.
19 Jul 2013
Without Screening Alcohol Abuse May be Missed
Patients come into a doctor’s office and give their symptoms to the doctor. The doctor listens, nods his head, and starts to piece together the symptoms the patient is mentioning and what he thinks may be the cause of those symptoms. But sometimes the patient doesn’t share everything with the doctor and the doctor does not ask some questions that could determine the causes or aggravations of an illness.
A new study from the School of Medicine at The University of Texas Health Science Center in San Antonio reveals that some questions doctors may not be asking are related to alcohol consumption. The article, in the Annals of Family Medicine, states that doctors may miss alcoholic symptoms in three out of four patients who come into their office.
 Screening Can Provide Proper Treatment
Screening Can Provide Proper Treatment
Researchers at UT Medicine conducted a study to see how well physicians could identify patients that exhibited symptoms of alcohol abuse. Over 1,600 participants were gathered from 40 primary care practices across multiple central states.
After participants were asked questions about their drinking habits, doctors were asked to make a diagnosis of whether or not the person was at risk for alcohol abuse. Participants were asked about the frequency that they drank alcohol and whether or not their drinking caused them to be reckless to themselves or with others. Doctors then categorized them in different alcohol use groups, including non-harmful drinker or harmful drinker.
Study co-author, Dr. Barbara Turner, stated that a doctor’s hunch missed identifying three out of four participants at risk for alcohol abuse. When doctors did suspect a person might be abusing alcohol though, the doctor was usually right.
Excessive Alcohol Consumption Hurts in Many Ways
Study authors believe that if patients were screened for their drinking habits that doctors may be able to help treat much more than alcoholism. High blood pressure, diabetes, liver disease, and some cancers have been connected to excessive drinking of alcohol. The 2011 National Health Interview Survey stated that over 85,000 people die each year from a circumstance where alcohol was misused.
Earlier studies reveal that when doctors have been able to identify harmful alcohol consumption habits in their patients, their patients decreased their alcohol consumption and improved their lives. Doctors provided brief counseling sessions to help their patients succeed in alcohol reduction.
Changing Procedures
Doctors can only treat what they see that needs to be treated. A screening procedure to help them identify a patient’s possible problems with alcohol use may help them better fully treat their patient.
Dr. Turner suggests that doctors screen their patients regularly to identify any changes in their drinking habits. A person may start drinking more heavily after both good and bad times like the following:
- Divorce
- Death of a loved one
- Loss of a job
- A new job or promotion to be social with new colleagues
- Celebrating with friends
If doctors catch harmful drinking patterns early, they may help prevent risky actions and future health problems in their patients.
Narcissism is a term psychologists and psychiatrists use to describe the combined presence of personality traits such as self-absorption, grandiosity, and an unrealistic sense of personal importance. Some aspects of narcissism can play a healthy role in a person’s life, while other aspects tend to produce social and interpersonal problems. In their worst form, narcissistic traits can manifest as a diagnosable mental health condition called narcissistic personality disorder. According to the results of a multi-university study published in 2012 in the journal PLOS ONE, narcissism produces significantly more negative health effects in men than it produces it women.
Narcissism Basics
Most psychologists and psychiatrists agree that a limited amount of narcissism can play a positive role in a person’s everyday life, both during the developmental stages of childhood and later on during adulthood. Experts in the field sometimes refer to this positive influence as adaptive narcissism. People who engage in adaptive narcissism can receive such benefits as an increased tendency to exercise, improved academic performance, an improved rate of recovery in the aftermath of a traumatic injury, improved or broadened employment opportunities, self-sufficiency in intimate relationships and improved parenting skills.
While adaptive narcissism can be beneficial on both a personal and social level, unlimited or maladaptive narcissism can have the opposite effect. Tendencies associated with unhealthy narcissism include an inability to hear the concerns of others, lack of empathy for others, an inability or unwillingness to take responsibility for one’s actions, an inability or unwillingness to take responsibility for one’s emotional states, and an unusual sensitivity to real or perceived criticism. The authors of the study in PLOS ONE break narcissism down into five personality traits, three of which tend to produce healthy narcissism and two of which tend to produce unhealthy narcissism. The three traits associated with healthy narcissism are self-absorption/self-admiration, leadership/authority and superiority/arrogance. The three traits associated with unhealthy narcissism are entitlement and exploitativeness.
Narcissism in Men
After reviewing their results, the authors of the study concluded that men and women with high scores for healthy or adaptive narcissism don’t experience significant increases in their cortisol levels. This finding indicates that adaptive narcissism does not produce stress. However, men with high scores for unhealthy narcissism do experience significant cortisol increases, and therefore experience substantial increases in their stress levels. In line with this finding, the highest levels of cortisol elevation occur in men who have the highest level of involvement in unhealthy narcissism. Interestingly, women with high levels of unhealthy narcissism experience less than half of the cortisol elevation that occurs in their male counterparts.In the study published in PLOS ONE, researchers from the University of Michigan and the University of Virginia used a 40-question questionnaire to determine the narcissism levels in a group of 106 adult undergraduate students. They also used saliva tests to check these students’ levels of a substance called cortisol. Cortisol is the body’s most important stress hormone, and when its level in the body increases, affected individuals experience mental symptoms of stress such as fear and anxiety, as well as a variety of physical stress-related effects.
Significance
Chronic stress is associated with increased risks for such things as depression, memory problems, sleep disturbances, obesity and heart disease. The men and women who participated in the study published in PLOS ONE did not undergo any stress-increasing experiments before having their cortisol levels checked. Instead, their cortisol levels reflected the amounts of stress they experience during everyday life. The authors of the study believe that this fact indicates that men with unhealthy forms of narcissism are regularly exposed to unique risks to their mental and physical well-being.
Social stereotyping may help explain the negative impact of unhealthy narcissism in men, the authors of the study note. For example, many of the common social definitions for “manliness” coincide with the personality traits of narcissism. If any given man with generally healthy narcissistic traits tries to live out the social expectations for males, he will probably not suffer any major negative consequences. However, if a man with generally unhealthy narcissistic traits tries to live out the same set of expectations, he can reinforce his damaging narcissistic behaviors and end up dangerously boosting his stress levels. As plausible as this sounds, it’s currently just a theory. Researchers will need to make additional studies before they can truly explain why unhealthy narcissism has such a strong impact on men.
04 Mar 2012
United Nation Estimates Drug Trafficking in West and Central Africa to Generate $900M Annually
The United Nation Office on Drugs and Crime (UNODC), estimates that cocaine trafficking is generating an enormous amount in drug trafficking to West and Central America and are then using the shortest route to Europe to transport them. The U.N. Security Council was recently told by the UNODC that West Africa is seeing a large increase in arms and human trafficking as well as piracy.