There are many negative consequences associated with drinking alcohol at a young age. Teens can suffer serious and immediate consequences after drinking alcohol, such as injury, engaging in dangerous sexual behaviors that can result in unplanned pregnancy or contracting a sexually transmitted disease. Or, they may choose to ride with a driver who is under the influence.
There are long-term effects, as well. Teens who drink are increasing their risk of developing heart disease or various types of cancer later in life. Because they begin drinking at a young age, teens expose their bodies to these risks for a longer period of time than a person who begins drinking in adulthood.
One major consequence of drinking is that it affects many other behaviors. Individuals who drink alcohol often experience a problem with executive functioning in the brain. Such brain functions as working memory are impacted by the consumption of alcohol.
The research about how alcohol affects executive function is often limited by the methods used to gather data. Often, researchers gather information about alcohol’s effects by asking participants to recount their experiences with alcohol consumption. This method carries with it all the potential problems inherent in data that relies on self-report, such as participants concerned about self-preservation or who remember events incorrectly.

Alcohol-Related Teen Behavior
Another method of examining alcohol-related behaviors is achieved through setting up an environment that mimics a real-life situation. Participants may be evaluated while they sip alcohol at an imitation bar or in a mock social situation. However, researchers cannot be certain that their imitation is close enough to the real thing.
A recent study by researchers at Rutgers University avoids the potential pitfalls of these types of studies by examining the impact of alcohol on executive functioning among students consuming alcohol in real situations. The study is unique in its consideration of the acute effects of alcohol on drinkers under the age of 21.
Previous studies have documented the effects of alcohol functioning, but the studies were focused on adults. The researchers wanted to measure the acute and chronic effects of alcohol on brain functioning in teens. These functions included such aspects as working memory and mental flexibility.
The researchers used field recruitment methods to gather data on underage drinkers, measuring intoxication levels through breath alcohol content. They also looked at chronic alcohol use by measuring the number of years the teen had been drinking.
The researchers used a “trail making test” to measure visuomotor performance and mental flexibility among 91 participants between the ages of 18 and 20.
The researchers found that the breath alcohol measurements were a predictor for performance on the trail making test. Those who had a higher level of intoxication performed more poorly on the task.
In addition, the researchers found that the current measurement of breath alcohol content and the measurement for chronic alcohol use predicted lower scores on the trail making test, but each predicted lower scores for different types of trails.
The research suggests that chronic alcohol consumption has a serious impact on the executive functioning processes of the brain among underage drinkers.
The information provided by the study highlights the potential that teens have for making significant mistakes while engaging in risky behavior after drinking. Teens may make poor decisions due to a low level of mental flexibility and visuomotor impairment.
By measuring the ability of teens to complete the trail making test in a field setting, the researchers were able to accurately measure how executive functioning works in a real-life setting for teens. The findings clearly indicate the danger involved for teens when they drink and then are faced with a risk-taking situation. The executive functioning required to skillfully navigate a risky challenge may not be present once alcohol has been consumed.
To Read More About The Dangers Of Addiction And Teenagers – Click Here
On May 14, 1988, a drunk driver going the wrong way on an interstate highway just outside Carrollton, Kentucky, collided head on with a school bus full of children. In total, 24 children and three adults were killed in this horrific accident, making it the most deadly alcohol-related automobile crash in U.S. history. In commemoration of the 25th anniversary of this tragic event, on May 14of this year the National Transportation Safety Board issued a new report urging all 50 states to lower the legal limit of intoxication for anyone operating a motor vehicle from .08 blood-alcohol content to .05, a standard that is already in place in about 100 other countries around the world.
Referring to the approximately 10,000 deaths that occur in the United States each year in alcohol-related automobile accidents as “a national epidemic,” NTSB Chairman Deborah Hersman expressed her organization’s concern that the ongoing campaign to reduce drunken driving fatalities had reached a point of diminishing returns. The NTSB’s recommendation that blood-alcohol level restrictions for drivers be tightened is in accordance with the latest scientific findings, which show that a person with a BAC of .05 will experience “reduced coordination, reduced ability to track moving objects, difficulty steering, and reduced response to emergency driving situations” (quoted from a chart published by the National Highway Traffic Safety Administration). The NTSB estimates that if this new standard were universally adopted, it could lead to a 10 percent annual decrease in the number of people killed by drunken drivers, and it is urging the National Highway Traffic Safety Administration to offer financial incentives to any state that will agree to make the switch from .08 to .05.
Sensible Caution or Mindless Prohibition?
 As recently as the early 1980s, people who had been drinking were legally allowed to get behind the wheel of an automobile in many states as long as their blood-alcohol content did not rise above .15. But in response to rising public and political awareness of the true costs of drunk driving, legal standards began to evolve and by 2004 all 50 states had adopted the far more stringent .08 standard that still reigns supreme today. Since the heyday of .15, annual casualties from alcohol-related automobile accidents have dropped from 20,000 per year to just under 10,000, but drunken driving still accounts for about one-third of all highway deaths in the United States, more than any other single factor. Over the years, legal penalties for driving under the influence have become more severe in concurrence with the tightening of the BAC, and bars, clubs, and restaurants by all accounts have become more responsible about serving alcohol to customers who may be intoxicated. Nevertheless, drunk driving has remained stubbornly and discouragingly prevalent, and its consequences have continued to leave a long trail of broken bodies lying in the wrecked and smoldering ruins of crashed automobiles each and every year.
As recently as the early 1980s, people who had been drinking were legally allowed to get behind the wheel of an automobile in many states as long as their blood-alcohol content did not rise above .15. But in response to rising public and political awareness of the true costs of drunk driving, legal standards began to evolve and by 2004 all 50 states had adopted the far more stringent .08 standard that still reigns supreme today. Since the heyday of .15, annual casualties from alcohol-related automobile accidents have dropped from 20,000 per year to just under 10,000, but drunken driving still accounts for about one-third of all highway deaths in the United States, more than any other single factor. Over the years, legal penalties for driving under the influence have become more severe in concurrence with the tightening of the BAC, and bars, clubs, and restaurants by all accounts have become more responsible about serving alcohol to customers who may be intoxicated. Nevertheless, drunk driving has remained stubbornly and discouragingly prevalent, and its consequences have continued to leave a long trail of broken bodies lying in the wrecked and smoldering ruins of crashed automobiles each and every year.
Not surprisingly, the alcohol and hospitality industries have responded to the .05 recommendation negatively, calling it unnecessary, excessive, and bad for the economy. Others have pointed out that current laws already allow police officers to arrest drivers who appear intoxicated regardless of what their blood-alcohol levels might be, and they claim that the only people who will be taken into custody under these new restrictions will be those with BACs of .05 who show no actual signs of being impaired. Even some people involved in the fight against drunk driving have expressed skepticism about the idea of reducing the allowable BAC, believing that it will create a backlash that may ultimately hurt the anti-drunk driving cause by linking it to draconian laws that will not be popular with most people. Skeptics also argue that this new law would be all but unenforceable, since police would be expected to somehow know intuitively that drivers had reached the legal limit for intoxication and needed to be pulled over, even though in most cases their driving performances would appear to fall entirely within the range of normal.
The Power of Prevention
Some of these criticisms could very well prove to be legitimate, if the new standards are eventually adopted. However, government regulatory and safety agencies can only base their policies and recommendation for change on what the latest research shows, and in this case the science is clear: at .05 BAC the reflexes and perceptions of human beings are altered dramatically, and regardless of whether a person shows obvious signs of drunkenness, their ability to drive will be impaired if they have been drinking enough to reach this level of intoxification, thereby putting themselves, their passengers, and everyone else on the roadways at risk. While there may indeed be some backlash in the short-term against a move to .05, if there is any chance at all that such a move will discourage drinking and driving then this new proposal by the NTSB clearly has merit.
During the time when BAC driving requirements were being progressively tightened, from approximately 1980 through 2004, drunken driving-related casualty levels declined significantly and no one can reasonably argue that this is just a coincidence. Based on past precedent it appears very likely that these new recommendations will in fact be adopted at some point, and if and when that happens we can only hope that from then on fewer families will be forced to confront the premature loss of cherished loved ones as a result of a tragic—and entirely preventable—alcohol-fueled automobile crash.
19 Jul 2013
Without Screening Alcohol Abuse May be Missed
Patients come into a doctor’s office and give their symptoms to the doctor. The doctor listens, nods his head, and starts to piece together the symptoms the patient is mentioning and what he thinks may be the cause of those symptoms. But sometimes the patient doesn’t share everything with the doctor and the doctor does not ask some questions that could determine the causes or aggravations of an illness.
A new study from the School of Medicine at The University of Texas Health Science Center in San Antonio reveals that some questions doctors may not be asking are related to alcohol consumption. The article, in the Annals of Family Medicine, states that doctors may miss alcoholic symptoms in three out of four patients who come into their office.
 Screening Can Provide Proper Treatment
Screening Can Provide Proper Treatment
Researchers at UT Medicine conducted a study to see how well physicians could identify patients that exhibited symptoms of alcohol abuse. Over 1,600 participants were gathered from 40 primary care practices across multiple central states.
After participants were asked questions about their drinking habits, doctors were asked to make a diagnosis of whether or not the person was at risk for alcohol abuse. Participants were asked about the frequency that they drank alcohol and whether or not their drinking caused them to be reckless to themselves or with others. Doctors then categorized them in different alcohol use groups, including non-harmful drinker or harmful drinker.
Study co-author, Dr. Barbara Turner, stated that a doctor’s hunch missed identifying three out of four participants at risk for alcohol abuse. When doctors did suspect a person might be abusing alcohol though, the doctor was usually right.
Excessive Alcohol Consumption Hurts in Many Ways
Study authors believe that if patients were screened for their drinking habits that doctors may be able to help treat much more than alcoholism. High blood pressure, diabetes, liver disease, and some cancers have been connected to excessive drinking of alcohol. The 2011 National Health Interview Survey stated that over 85,000 people die each year from a circumstance where alcohol was misused.
Earlier studies reveal that when doctors have been able to identify harmful alcohol consumption habits in their patients, their patients decreased their alcohol consumption and improved their lives. Doctors provided brief counseling sessions to help their patients succeed in alcohol reduction.
Changing Procedures
Doctors can only treat what they see that needs to be treated. A screening procedure to help them identify a patient’s possible problems with alcohol use may help them better fully treat their patient.
Dr. Turner suggests that doctors screen their patients regularly to identify any changes in their drinking habits. A person may start drinking more heavily after both good and bad times like the following:
- Divorce
- Death of a loved one
- Loss of a job
- A new job or promotion to be social with new colleagues
- Celebrating with friends
If doctors catch harmful drinking patterns early, they may help prevent risky actions and future health problems in their patients.
Pain medications are often prescribed for chronic pain related to other medical conditions, such as cancer or an injury that results in ongoing pain. In all cases, the prescription of a pain medication to relieve pain must be weighed against the potential negative consequences of using such a medication, including not only side effects but also the risk of addiction.
In addition, the pain is best managed when there are follow-ups to the prescription that include assessments of pain levels and examination of co morbid conditions. In a recent study, researchers led by Leslie R.M. Hausmann, PhD of the Veterans Affairs Pittsburgh Healthcare System and Assistant Professor of Medicine at the University of Pittsburgh discovered that there are significant disparities between races in how pain management is executed.
The researchers found that the differences are present in the monitoring of opiods and in the follow-up routines. The recommended guidelines include assessing patients for the effectiveness of the medication, as well as screening them for evidence of drug abuse. The study’s findings appear in a recent issue of the journal PAIN.
The study’s focus included several measurements of pain management defectiveness, including the physicians’ implementation of an opioid agreement, measurement of pain levels at follow-up exams, inclusion of urine screenings for drugs and referrals for pain clinics and substance abuse treatment.
The retrospective design incorporated health records representing 1,646 white patients and 253 black patients. The data was taken from electronic health records that met certain criteria. The patients were all prescribed opioids for pain not related to cancer at the Veterans Affairs Pittsburgh Healthcare System pharmacy and used the medication for at least 90 days. The records were all from October 2007 to September 2009.
The researchers also assessed data about prescription painkiller follow-up and monitoring practices for the 12 months following the prescription period, to form a complete profile of the pain treatment.
The patients were 94 percent male and 22 percent were over the age of 65. Forty-five percent were married or living with a partner, and were most commonly treated for joint or back pain. Approximately one half of the patients had a co morbid mental or physical health condition, and one-third of the patients had a past of substance abuse.
 When comparing the patients, the black patients were younger, less liable to have pain in their back, and had more physical co morbidity and higher pain levels recorded. The black and white patients were similar in history of drug abuse.
When comparing the patients, the black patients were younger, less liable to have pain in their back, and had more physical co morbidity and higher pain levels recorded. The black and white patients were similar in history of drug abuse.
However, major racial differences were discovered as pertained to monitoring of pain prescription use and the effectiveness of the medication. Black patients seemed less likely to be monitored for pain levels during medical exams and among those patients given a urinalysis, black patients were tested more often, and particularly if they were prescribed a higher dose of medication.
Black patients also were less liable to receive a referral to a specialist for pain treatment and were more likely referred to a substance abuse treatment facility after taking prescription opioids.
The findings indicate that when black patients are prescribed opioid medications for pain treatment, they may not be receiving similar follow-up and monitoring practices that may maximize the benefit of their pain management treatment.
Read more about Dispelling Racial and Socioeconomic Myths About Drug Users
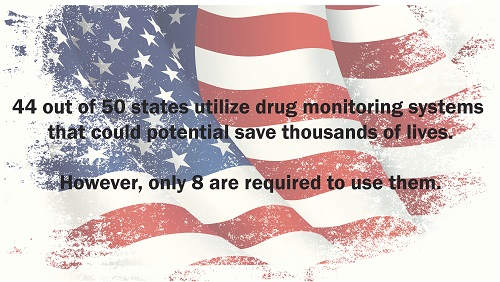
Many state legislatures have enacted laws to make it easier for them to establish a prescription database to track drug abuse. These programs are often put in place to assist law enforcement in cracking down on illegal activity such as producing methamphetamine. Clandestine laboratories rely on large amounts of cold medicine to produce their dangerous substances that wreck lives. Most of that activity has been squelched by drug monitoring programs; another advantage to these programs affects more than just law enforcement.
The monitoring programs also help point the way to users who are likely abusing a prescription drug, which can lead interventions that are potentially life saving. These programs, which are now up and running in 44 states, have proven to be an invaluable tool for healthcare providers. They are now able to legally monitor the frequency of prescription drug use among their patients. The drugs being monitored include opioids, amphetamines and sedatives. But laws vary per state and only eight states currently require providers to participate in the monitoring programs.
What is certain is that the states that do allow a monitoring program have less of a problem with the current epidemic of pain killer abuse in this country. While not much is known about how the monitoring programs are affecting the way doctors prescribe their drugs, one study done in Ohio shows that more than 40 percent of emergency room doctors who had access to their patient’s prescription drug history made different prescription decisions based on the data from the monitoring program.
Almost all physicians are pressed for time, which means their ability to thoroughly study the data available to them is hampered. Furthermore, the amount of resources available to healthcare professionals to fully interpret the data providing by monitoring programs is also in short supply, limiting the impact that the data could have on the health of patients across the nation.
11 Jul 2013
Relapse Prevention: Study May Have Found Key to Preventing Stress From Triggering Relapse
For the person who has fought back against drug addiction and has been walking the road of recovery, stress can pose a dangerous threat. For many, the stress of struggling to find work, rebuild relationships, or a sudden loss through death can be enough to trigger a return to using drugs. Stress is a powerful force for people without an addiction history, but when there has been a pattern of soothing stress with substances, the temptation to do so again when the stress temperature rises is great. A recent National Institutes of Health-funded study may have discovered the key to preventing stress from triggering that kind of relapse.
The grant-funded study was actually a partnership between researchers from the University of Pennsylvania and Brown University. The investigation provides a clear outline for the sequence of events within the brain leading up to a stress-induced drug relapse. The study debunked prior hypotheses about the relapse pathway and uncovered evidence that the part of the brain connected to meeting basic needs (the VTA) was pivotally involved.
The study employed rats with a history of cocaine addiction but who were not presently addicted. Some of the rats were treated with a chemical (nor-BNI) that inhibits certain VTA receptors (known as kappa opioid receptors), while the other group of rats did not receive the treatment. Next, all of the rats were made to undergo five minutes of stress-inducing exercise. Observation showed that the treated rats did not revert to cocaine use even after being stressed. The non-treated rats did go back to cocaine.
When we meet our body’s essential needs such as eating and drinking, the brain releases dopamine, a chemical that rewards our behavior with a sense of pleasure. At the same time, healthy brains also release GABA, which modulates dopamine release. Drugs keep GABA from doing their job of controlling the dopamine flow and hence drug use produces an oversized rush of good feelings.

Relapse Prevention with Stress Prevention
In this study, researchers first demonstrated that stressors prevent GABA from slowing down dopamine release. This explains how stress can be a preamble to drug relapse. In the presence of stress, the proper amounts of reward chemicals are disordered. Pleasurable activities become inordinately pleasurable. However, the study team showed that by introducing nor-BNI into the VTA area of the brain, the dopamine controls remained in place even during periods of stress.
By honing-in on the neural underpinnings of a stress-caused relapse, these scientists may have found a way to interrupt the chain reactions that trigger a return to drug use. The study could prove to be a major leap forward toward creating a targeted medication that could remove a domino from the stack and prevent the inevitable result.
Finding a rehab that has not only a great rehabilitation program but a great aftercare program is another way to help prevent relapse. Read Choosing the Right Drug Rehab for Your Loved One to learn more.
Reporting the news in Mexico can be a deadly occupation, especially for those covering the drug war. But where militant thugs have been successful in stifling the media, they are virtually powerless against those who have taken to social media to “report” the war.
It’s not only Mexican residents caught in the crossfire taking to Twitter, YouTube and Facebook, those across the border in the U.S. are also using social media as a tool. Residents are using social media to protect themselves from the drug cartels that stop at nothing to push their product and protect their turf.
 The violence began in earnest when the Mexican president declared war on drugs, but crept up another few notches when two major partnering cartels split and declared war on each other. Since the declarations of war, it is estimated that as many as 100,000 people have been killed and another 30,000 have seemingly vanished into thin air. Many residents try to escape the most violent areas, which has put more than 200,000 in a displaced status.
The violence began in earnest when the Mexican president declared war on drugs, but crept up another few notches when two major partnering cartels split and declared war on each other. Since the declarations of war, it is estimated that as many as 100,000 people have been killed and another 30,000 have seemingly vanished into thin air. Many residents try to escape the most violent areas, which has put more than 200,000 in a displaced status.
Some of the only news sources available now are through Twitter and Facebook. While news footage once came from the major broadcast companies in Mexico, camera phones with crudely edited footage of the war between the government and the cartels is being placed on YouTube instead. Media outlets in the U.S. are also depending on these amateur videos as their go-to source for footage.
America’s ongoing drug dependency is fueling this war. About 90 percent of illicit drugs making their way into the U.S. are coming through Mexico. The biggest cash crop, so to speak, continues to be cocaine.
According to the National Institute on Drug Abuse, nearly 5 million Americans said they had at one point or other abused cocaine. While those numbers pale in comparison to the drug’s peak in 1982 (10.5 million were believed to be using the drug in that year), it’s still enough to fuel a drug war that is taking lives.
Read more: United Nations Leading International War on Drugs
Curbing drug use isn’t something that can be solely dealt with at a national level. Effective policies must be put in place on a global scale. In 2010, approximately 5 percent of people all over the world, or 230 million individuals, admitted to engaging in illegal drug use at least once.
 The United Nations Office on Drugs and Crime (UNODC) has been working since 1961 to control drug use in order to preserve public health and welfare. Each year, illegal drugs claim the lives of around 200,000 people. So many of these individuals might not have had to die had they received the help they needed.
The United Nations Office on Drugs and Crime (UNODC) has been working since 1961 to control drug use in order to preserve public health and welfare. Each year, illegal drugs claim the lives of around 200,000 people. So many of these individuals might not have had to die had they received the help they needed.
Since its inception, the organization has made an effort to combat this issue not only with law enforcement, but also with policies that would address the deeper core issues of health and addiction.
According to Reuters, the UNODC global drug conventions that took place in 1961, 1971 and 1988 have helped standardize the world’s drug regulation policies, reducing the proliferation of illegal drugs. In fact, even as the world’s population has continued to multiply over the last hundred years, global production of opium, for instance, has decreased by 80 percent.
Many individuals addicted to drugs are sick and do not belong in a prison with hardcore criminals. While there are those who would say that legalizing drugs is the answer to combat the international drug problem, proponents of the UNODC efforts say that current measures are working.
But for these measures to continue being effective, countries around the world must offer education, rehabilitation, and social reintegration programs to drug offenders rather than prison sentences. Receiving these individuals as patients instead of criminals presents the greatest opportunity for change so that everyone has the chance to lead a healthy life free from drugs and crime.
Drugs available in your backyard? Teens say drugs easy to get their hands on in New Mexico.