A new drug that has devastating consequences for its users may have finally been confirmed to have made it into the U.S. The drug is called Krokodil, and it first appeared in Russia as a cheap, homemade substitute for heroin. The name, which means crocodile in Russian, refers to the scaly sores that appear almost immediately after using this drug. The sores begin under the skin and can be so bad that the drug has been described as flesh-eating. The result is horrific and can lead to scarring, amputation, and even death.
Krokodil Beginnings In Russia
 Homemade injectable opioid drugs are nothing new in Russia. Resourceful people there have been creating and using their own drugs to get high for decades. In the 1990s, the heroin trade from Afghanistan increased and drug users did not need to make their own substitutes. Heroin addiction became a serious and widespread problem in the country.
Homemade injectable opioid drugs are nothing new in Russia. Resourceful people there have been creating and using their own drugs to get high for decades. In the 1990s, the heroin trade from Afghanistan increased and drug users did not need to make their own substitutes. Heroin addiction became a serious and widespread problem in the country.
Over the last few years, the Russian government has targeted illegal opium sales to try to solve the problem of heroin addiction. As sources of heroin dwindled and the product became more expensive, the practice of making heroin substitutes at home came back into favor. Krokodil is easily made from codeine, a prescription opioid, and other household chemicals.
Krokodil gives the user a high similar to heroin, but with even worse side effects. The green and black colored sores and ulcers begin to appear soon after the first use, and get worse as use of the drug continues. The drug, with the chemical name desmorphine, as well as the other chemicals that go into making it, tend to clump up and stay inside blood vessels all over the body. The clumps lead to infections and sores that spread and worsen.
Disputed Krokodil Cases In The U.S.
Experts in the field of illegal drugs have long feared that Krokodil would eventually show up in the U.S. Several disputed cases have been reported, including a doctor in the Chicago area who is convinced he treated two young women with the sores caused by Krokodil use. Cases in California and other states were also unconfirmed.
Reputable Case Of Krokodil Use In The U.S.
Now, it would seem that the worst fears of some have been vindicated. Two doctors working at St. Mary’s Health Center outside of St. Louis, Missouri, have published their findings from treating a victim of Krokodil use. They treated the 30-year-old man in December 2012. He had sores all over his legs. His skin was rotting away in places, and he had lost a finger on one hand to the infection. He told the doctors that he had been injecting himself with a synthetic heroin substitute that he made using codeine, gasoline, and other household chemicals. The admission, along with the sores, made a strong case that the doctors did treat a young man who had been using this scary new form of heroin.
Krokodile – Possible Future U.S. Epidemic?
If the doctors are right and Krokodil is now being used in the U.S., the implications are very serious. If drug users addicted to heroin and other opioids learn how to make this drug and can do so inexpensively, it could represent a new epidemic, much like what has been seen in Russia. The disfiguring effects of using Krokodil, as well as the addictive nature of the drug, mean that many people will suffer, and even die from using it. The Drug Enforcement Agency has yet to confirm the presence of Krokodil in the U.S., but with reports coming in from emergency rooms across the country, that confirmation does not seem to be far off.
Read More About Krokodil Claiming U.S. Victims
The 18th century British philosopher and statesman Edmund Burke once famously declared: “Those who don’t know history are destined to repeat it.” In the years since, Burke’s quote has been repeated often in slightly different forms by a variety of public figures, which is a testament to how much truth the sentiment behind it contains.
 This statement could undoubtedly be applied quite aptly to the ongoing War on Drugs. Over the past several decades United States law enforcement agencies have spent over $1 trillion persecuting this war, and during that time hundreds of millions of tons of illegal drugs have been seized and destroyed here and around the world. And yet, much to the chagrin of those responsible for the continuation of this military-style anti-drug campaign, there is no evidence to suggest that any drug pipelines have been permanently closed off or that the flow of illegal substances has been reduced in any meaningful way as a result of this approach. In fact, the international drug trade appears to be more profitable and efficient than ever before.
This statement could undoubtedly be applied quite aptly to the ongoing War on Drugs. Over the past several decades United States law enforcement agencies have spent over $1 trillion persecuting this war, and during that time hundreds of millions of tons of illegal drugs have been seized and destroyed here and around the world. And yet, much to the chagrin of those responsible for the continuation of this military-style anti-drug campaign, there is no evidence to suggest that any drug pipelines have been permanently closed off or that the flow of illegal substances has been reduced in any meaningful way as a result of this approach. In fact, the international drug trade appears to be more profitable and efficient than ever before.
Effects Of Drugs On The Black Market
The Sept. 30 edition of the online medical journal BMJ Open includes a report from a multi-national team of researchers who studied and analyzed international drug surveillance databases in order to identify long-term trends in the illegal drug trade. They discovered that despite the stalwart anti-drug efforts of law enforcement, officers and administrators from across the globe, over the last 20 plus years the cocaine, heroin and marijuana available on the international black market has gotten both stronger and less expensive.
In the United States, from 1990 to 2007 the potency of these three substances rose by 60 percent, 11 percent and 160 percent respectively, and yet the street price of these three popular illegal drugs actually fell by 80 percent over the same time period when adjusted for inflation. The increased strength of such drugs is a testament to the fact that demand for illegal substances has remained high enough to spur constant innovation in production methods, while their steadily dropping price shows that supplies are bountiful and that users of cocaine, heroin or marijuana are still very much operating in a buyer’s market.
War On Drugs And Illegal Drug Use
Contrary to hype and popular opinion, the War on Drugs was never designed to stop the trade of illegal substances entirely. Instead, its goal has been to disrupt supply chains just enough to drive prices up and make dangerous intoxicants unaffordable to many who might be tempted to experiment with them. But even this modest goal has proven elusive, and few if any honest observers still believe that ramped up law enforcement strategies will ever reduce illegal drug consumption or prevent millions of users from plunging headfirst into the dark canyon of substance abuse and addiction.
At the present time, the global black market drug trade generates about $350 billion in tax-free profits annually. In the U.S. alone, there are approximately 22 million illegal drug users above the age of 12, and while the majority could not accurately be classified as addicts, those who do become dependent on substances like cocaine, heroin and methamphetamine usually have no difficulty in obtaining the supplies they need to quench their addictive thirsts. And with drugs becoming stronger and cheaper, we may start seeing greater percentages of casual drug aficionados eventually succumbing to addiction, since these individuals will be able to afford greater quantities of illegal substances even as the high they are getting from what they are using intensifies.
Drug Popularity, Reputation And Availability
It is true that the rates of usage of drugs such as cocaine, angel dust and heroin have generally been declining over the years. However, it would be a mistake to assume that the drug war has been successful just because certain drugs have now gone out of style. Once a drug starts to get a bad reputation, its use will usually decline. But as some drugs become less popular, other illegal substances will inevitably flood the market to fill the void, and, as a result, the whole cycle of casual use, abuse, addiction and disillusionment just keeps repeating itself with no apparent end in sight.
What Can Help Drug Addiction?
We can only speculate about what might finally make the merry-go-round of drug dependency stop spinning—expanded availability of treatment, more drug courts, innovative educational campaigns, greater social awareness, a reduction in the rates of poverty and unemployment, community outreach programs, or some combination of all of the above. It seems clear, however, that more interdiction, indictment and incarceration will not make the decisive difference.
The “Just Say No” campaigns were mocked in their day and seem hopelessly quaint now. Trying to shame people into avoiding drugs has not worked any better than treating drug use as a crime. But in the end, illegal drug use will only decline precipitously if enough people decide the risk of addiction is too great to flaunt. So in a sense, it really is about just saying no, and being able to recognize the critically important reasons it is logical to do so. Cheaper and stronger means extreme danger, and consequently a refusal to get involved with drugs in the first place is the smartest decision one can make.
Continued From – How To Handle A Loved One With An Addiction – Part 1
No one is born with a set of instructions on how to handle an addict. My perspective on what tends to work and what doesn’t, or perhaps better said, what can be helpful and what definitely is not, is born of my own experience as an addict. When I was ready to recover, and when I wanted it because it was what I knew I needed, it mattered little what people had said or hadn’t said. Nonetheless, looking back, I can see that some approaches were helpful while others resulted only in resentments I had to later work through in recovery.
What Is Helpful When Dealing With An Addict
By labeling these ideas “helpful,” I do not mean to imply that they will achieve the desired result of getting the addict to get clean. It is rather to say that these approaches are less likely to do harm and are more likely to help maintain a relationship of trust between you and the addict. In the end, the addict has to choose recovery because she wants it—not because you do.
Give Space
Addicts are already isolators, so it may appear that all they want is more and more space and time to be alone and practice their addiction. By giving space, I mean to say, emotional space. Keep the addict near and continue to engage to the degree that she is able or willing. But refrain from making every conversation or occasion together about the disease. The addict already feels the all-pervasiveness of it. You don’t need to keep bringing it up or checking in.
Share The Struggle
Many families of addicts make the mistake of keeping the issue a secret. This failure to reach out is generally based in the fear of the stigma attached to addiction and mental illness. But you need support and help in what may be a very long battle. Start by speaking with a pastor at your church or with trusted family friends. You do not need to be ashamed, this is no one’s fault. Addiction is painfully isolating not only for the addict but for the family who has to live and deal with the secret problem as well. Humble yourself to bring others in for support.
Get Help For You
Addiction touches and traumatizes the lives of everyone in its midst. Family members and even friends can benefit from counseling or a series of Al-Anon meetings. Become educated about the disease and learn what you can and cannot realistically expect from an addict. Learn to recognize patterns of manipulation and become aware of your own potential tendencies for co-dependency and enabling. Find out how to set proper boundaries around a person with addiction and get the support you need in sticking to them. Programs like Al-Anon are miraculous in helping those who live with addicts to understand what their role is in dealing with an addict.
While I was blessed with recovery from my anorexia, I watched another young girl lose her life to it at the age of 24. If the addict you love does not find recovery, you must not blame yourself. You cannot save someone who will not be saved. By the same token, you cannot, even by poorly chosen words and unthinking behavior, stop someone from seeking recovery and getting well if that is what they have decided to do.
There is no easy way to approach, handle or talk to a loved one struggling with addiction.
If you have an addict in your life, expect it to be difficult, awkward and uncomfortable. There will be good days and bad days, there will be small successes followed by perhaps greater setbacks. You will be pushed to your emotional limit and you will be forced to face your own inability to change a person you love. You will be wholly incapable of making him see that what you want is what’s best for him.
Helping Those Dealing With Addicts
Dealing with addicts isn’t intuitive. We don’t simply discern how to get through to them or how to interact with them based on common sense or reason. While respecting addicts as people, it will help the non-addicts in their midst to understand that reason, good sense, morality and self-preservation are no longer part of a framework within which they operate or a common ground upon which to meet.
But that doesn’t mean we write addicts off as crazy and give up hope. Having been an addict myself, I had a lot of people around me trying to help or cure or fix me in different ways. From the vantage point of recovery, I can now look back and comment on what was helpful and what wasn’t. Even a decade later, I remember how the people around me treated me when I was drowning in the despair of my addiction. While nothing you say will make or break an addict’s chances of recovering, there are ways of communicating and interacting that are harmful and pain-inducing, and there are better, more helpful ways of trying to relate to a person who is indeed quite sick.
What Not To Do When Dealing With An Addict
Guilt Trips
Yes, the addict is making everyone’s life difficult and causing a lot of unnecessary pain and suffering. She breaks plans, she fails to keep her commitments, she is unreliable and unpredictable. And guess what: she already knows it. Asking things like, “Do you realize what you are doing to your mother?” or, “Don’t you understand how you are hurting us?” are not helpful. The addict, though selfish in the extreme, is not oblivious to the pain, difficulty and chaos she is bringing into the lives of those around her. But she is not able to stop it. A guilt trip presupposes that the person being guilted is acting deliberately or out of malice. It assumes that he or she has some control over the offending behavior. An addict does not.
Bargaining
You’ll do anything, make any promise, as long as the addict will agree to stop the addiction and get help. But the addict is powerless to take you up on that offer. The addiction is boss. As appealing as your offer might be, it simply isn’t possible. Addicts are known for high-stakes gambling. They gamble their families, their jobs and anything good they can claim. They know what they have to lose and they do it anyway. They don’t do it because they don’t care; they do it because the illness is in fact that powerful and enslaving.
Endless Pleading And Cajoling
This is also known as nagging and it is never helpful or effective. It’s not that the addict doesn’t care, it’s that she cannot stop what she is doing on the basis of your wishes—even if she wanted to. The disease is a lot stronger than that. It’s a lot stronger than she is. In the end, the addict may tell you what you want to hear, but then go back to business as usual. She knows you think there is a problem. You don’t have to continue to restate it.
Implying Fault Or Agency
Loved ones must burn into their minds that both substance and process addictions are not choices that the addict is making. As a result, blaming addicts or implying that they are practicing their addiction simply because they are selfish and unloving is not only incorrect, but cruel. Understand that the addict is in the grip of something much bigger than him or herself. Addiction is an illness like diabetes or cancer. You may hope that addicts will take the appropriate steps to manage the condition, but it is unhelpful to imply that they do what they do on purpose.
Ignoring The Issue
If there is nothing that can be said to make an addict want to seek help, and if the nagging and the pleading are ineffective, does that mean it’s better to say nothing at all? Is it better to ignore the issue, make the best of it or hope it all just goes away? No. Something does indeed need to be said and maybe even done, but the ways in which you speak and act hold the difference between showing genuine love and support, and being a nuisance and a nag.
While your words and expressions of concern may not effect immediate change in the addict’s life, while they may not leave your chat promising to check into treatment, the addict will benefit from the knowledge that you cared enough to say something out of concern and love. Don’t pretend there isn’t a problem.
Continued In – How to Handle A Loved One With An Addiction – Part 2
20 Sep 2013
Understanding Opioid-Related Disorders
Opioid-related disorders is the collective name of a group of substance-related disorders listed in the Diagnostic and Statistical Manual of Mental Disorders, a reference guide commonly used by mental health professionals across America. All of the conditions with this name involve negative consequences associated with the use of a wide variety of opioid narcotic medications or drugs. DSM 5, the 2013 edition of the Diagnostic and Statistical Manual, makes several changes to the definitions of the opioid-related disorders. Some of these changes involve a mere change in wording, while others involve a significant change in meaning.
Opioid-Related Disorder Basics
The five opioid-related disorders listed in DSM 5 are opioid use disorder, opioid intoxication, opioid withdrawal, “other” opioid-induced disorders and “unspecified” opioid-related disorder. Opioid use disorder is a new condition created by blending the definitions for two other conditions, called opioid abuse and opioid dependence, which appeared in the “Diagnostic and Statistical Manual’s” obsolete fourth edition (DSM IV). Opioid intoxication and opioid withdrawal keep the same definitions they had in DSM IV. The “other” opioid-induced disorders heading is a substitute for five separate DSM IV conditions. “Unspecified” opioid-related disorder acts as a substitute for a loosely defined DSM IV disorder called opioid-related disorder not otherwise specified (NOS).

Opioid Use Disorder
Opioid drugs and medications are well known for their ability to trigger substance abuse in users, as well as substance dependence (a medical term for addiction). People affected by substance abuse don’t meet the criteria for diagnosing a physical/mental addiction, but still participate in ongoing substance-based behaviors that strongly impact their lives in negative ways. People affected by substance dependence do meet the criteria for diagnosing an addiction; like substance abusers, they also participate in clearly harmful substance-based behaviors on a regular basis.
Issues of substance abuse and substance dependence overlap to a considerable degree. In fact, from a scientific standpoint, it’s perfectly reasonable to view dependence as a particularly damaging form of abuse. DSM IV kept the diagnosis of substance abuse and substance dependence strictly separated. However, DSM 5 discards the separate listings contained in DSM IV and establishes a replacement condition—called substance use disorder—which joins the symptoms of substance abuse with the symptoms of substance dependence. In accordance with this change, opioid users with significant abuse- or dependence-related problems will now receive a single diagnosis for opioid use disorder.
Opioid Intoxication
People in the midst of opioid intoxication develop at least two symptoms that alter their normal mental function, change their behavior for the worse, or otherwise impede their ability to carry out their typical routines. In all cases, one of the symptoms present must be unusual narrowing or widening of the pupils. Other qualifying symptoms include an inability to pronounce words properly, unusual sleepiness, a decline in normal memory function, a decline in the ability to voluntarily focus attention, and the onset of the dire state of unresponsiveness known as a coma. Additional requirements for a diagnosis include verifiable use of an opioid drug or medication in the very recent past and lack of other psychological or physical issues that could produce the problems attributed to opioid use.
Opioid Withdrawal
Opioid withdrawal occurs when an opioid user who has grown accustomed to the effects of a drug or medication suddenly stops using that drug or medication, or steeply decreases use over a short span of time. The Diagnostic and Statistical Manual provides doctors with guidelines to gauge the seriousness of withdrawal in any given patient. People going through grade 0 opioid withdrawal typically develop symptoms such as anxiety, a strong desire to continue drug/medication use, and the presence of behaviors designed to fulfill that desire. People going through grade 1 withdrawal develop symptoms such as unusual sweat output, uncontrollable yawning and unusual tear or mucus production. Symptoms associated with grade 2 opioid withdrawal include twitching muscles, restricted eating patterns similar to those found in people with anorexia, and pupil dilation. Grade 3 opioid withdrawal symptoms include sleeplessness, cramping abdominal muscles, muscle weakness, diarrhea, vomiting, and abnormal increases in blood pressure, heart rate and breathing rate.
“Other” And “Unspecified” Disorders
The “other” opioid-induced disorders diagnosis is designed to describe the presence of any mental disorder-related symptoms that appear as a consequence of opioid use. It replaces five separate diagnoses contained in DSM IV, including opioid-induced mood disorder, opioid-induced sleep disorder, opioid-induced sexual dysfunction, opioid-induced psychotic disorder with delusions, and opioid-induced psychotic disorder with hallucinations. The “unspecified” opioid-related disorder diagnosis lets mental health professionals identify cases of opioid-related mental health problems that don’t meet the minimum requirements for diagnosing any other opioid-related disorder.
The question of how we should deal with people with the brain disease of addiction isn’t an easy one. The criminalized approach, which would have drug users sitting in jail cells across the country and offers little in the way of medical help, has had its time in the sun. Putting people in jail accomplishes very little, with soaring re-arrest rates for drug crimes testament to the fact that merely punitive action is not enough to deal with the nation’s drug problem. This is the key idea behind drug courts — they aim to help drug users solve problems and get into treatment, rather than sending them straight to jail. Graduates of drug courts, like Melissa Swanger and Kathleen C., often become advocates for the approach, a testament to their ability to turn people’s lives around.
Introduction to Drug Courts
Drug courts are specialized courts for those addicted to drugs or alcohol. Rather than send people with recognized illnesses to jail over and over again, drug courts use a multi-pronged approach with the aim of reducing the chances of both relapse and re-arrest. They do this through interactions with a judge, treatment and rehabilitation services, monitoring, supervision, sanctions and incentives, all offered according to the individual’s requirements as determined by an initial risk and needs assessment. There are consequences for failure, however; if the individual continually relapses or commits crimes, the system effectively reverts to the ordinary, incarceration-based approach.
Melissa and Kathleen’s Stories
 Melissa Swanger had no criminal record until she started using meth. Her goal was to lose weight, but in addition to the 60 to 70 pounds, she lost a lot more, including her home, her car and her children as a result of her addiction. Because there was no indication she was a criminal before she began taking meth, her lawyers pointed her in the direction of the local drug court. Eight years after her entry into drug courts (and seven after her graduation) she is still clean, having made a lasting change in her life, rebuilt relationships and taken responsibility for her actions. She called it “the toughest blessing I’ve ever had,” and went on to comment how the drug court team is “willing to help people instead of saying just throw away the key.” The approach worked wonders for her, and she’s never looked back.
Melissa Swanger had no criminal record until she started using meth. Her goal was to lose weight, but in addition to the 60 to 70 pounds, she lost a lot more, including her home, her car and her children as a result of her addiction. Because there was no indication she was a criminal before she began taking meth, her lawyers pointed her in the direction of the local drug court. Eight years after her entry into drug courts (and seven after her graduation) she is still clean, having made a lasting change in her life, rebuilt relationships and taken responsibility for her actions. She called it “the toughest blessing I’ve ever had,” and went on to comment how the drug court team is “willing to help people instead of saying just throw away the key.” The approach worked wonders for her, and she’s never looked back.
Another story comes from Kathleen C., a mother who found herself committing crimes in order to fund her habit—which graduated from prescription drugs to heroin and meth—so she could use at all hours of the day. She started getting high at work and lost two jobs over the course of her addiction so that eventually she was only working “seasonally” so that employers didn’t catch on to her issues. Eventually, she was arrested for theft and forgery, a moment that became her turning point. After her three-month stretch, she asked to be sent to a drug court. Since then, she’s been clean, graduating in 2012 and managing to repair her relationship with her son. She fought the program at the beginning, but soon realized it was what she needed to overcome her addiction. Since graduating she has gotten engaged and has gained an associate’s degree in applied sciences. She says, “there’s a lot of beautiful things in my life today that I wouldn’t have thought possible.”
Becoming Advocates
After finishing the program, Melissa and Kathleen have become advocates for the drug courts approach. Melissa has become a recovery group leader with a church and tells her own story to inspire others to make a change. The passion the recent graduates show for the program is a testament to its ability to change lives, and the advocates it produces may lead others to make similar decisions to improve their day-to-day existence.
Punishment for Addiction: A Thing of the Past?
The drug court approach seems to be proving that the traditional, punishment-based strategy for dealing with addiction is fundamentally flawed, but not everybody shares the enthusiasm of recent graduates. There are stories of those for whom drug courts did not work, as well as critiques from groups like the Drug Policy Alliance, who argue that drug courts are not cost-effective and leave some people worse off than when they started and that the approach is more punitive than the previous method. This is because they punish users for relapsing, generally with jail time and ejection from the program, with harsher sentences for those who’ve been deemed “failures” in their attempts to get clean. However, whether this is an issue with drug courts as a concept or with how they’re put into practice is unclear.
On the other hand, the National Institute of Justice offers statistics indicating that drug courts are effective at reducing costs to the justice system (an average of $1,400 cheaper per participant) and reducing rates of re-arrest by up to 28 percent over the course of two years. The Drug Policy Alliance alleges that these studies are poorly conducted and often focus on less serious cases, but don’t deny the effectiveness of the approach for some users.
It’s unclear whether drug courts really are as effective as they’re reputed to be, but with the alternative being jail time with no real assistance in getting clean—they must be a step in the right direction. Perhaps a more health-centered approach would be even better, but these types of moves must be made gradually. Maybe, just maybe, the days of punishing people for a health problem are coming to an end.
The loved ones of an individual addicted to a destructive substance such as methamphetamine or heroin often watch, perplexed, as the addict destroys their life for a substance that makes them miserable.
A new study may help explain why addicts keep going back to a substance that produces an unpleasant consequence. Researchers at the University of Michigan recently uncovered clues to the change in motivation that often occurs in drug users as they become addicted by testing similar behaviors in animal models.
Read More
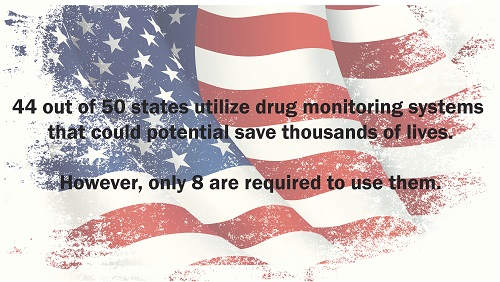
Many state legislatures have enacted laws to make it easier for them to establish a prescription database to track drug abuse. These programs are often put in place to assist law enforcement in cracking down on illegal activity such as producing methamphetamine. Clandestine laboratories rely on large amounts of cold medicine to produce their dangerous substances that wreck lives. Most of that activity has been squelched by drug monitoring programs; another advantage to these programs affects more than just law enforcement.
The monitoring programs also help point the way to users who are likely abusing a prescription drug, which can lead interventions that are potentially life saving. These programs, which are now up and running in 44 states, have proven to be an invaluable tool for healthcare providers. They are now able to legally monitor the frequency of prescription drug use among their patients. The drugs being monitored include opioids, amphetamines and sedatives. But laws vary per state and only eight states currently require providers to participate in the monitoring programs.
What is certain is that the states that do allow a monitoring program have less of a problem with the current epidemic of pain killer abuse in this country. While not much is known about how the monitoring programs are affecting the way doctors prescribe their drugs, one study done in Ohio shows that more than 40 percent of emergency room doctors who had access to their patient’s prescription drug history made different prescription decisions based on the data from the monitoring program.
Almost all physicians are pressed for time, which means their ability to thoroughly study the data available to them is hampered. Furthermore, the amount of resources available to healthcare professionals to fully interpret the data providing by monitoring programs is also in short supply, limiting the impact that the data could have on the health of patients across the nation.