10 Apr 2013
Tips for Coping with the Pressure to Relapse
Getting into rehab for your addiction was a huge and important step. Making it through the process was an uphill battle. Now, you are out of rehab and back in the real world. The first thing you want to do is drink, right? No matter what anyone tells you before you go into recovery, resisting the urge to relapse once you are sober may just be the hardest part of all.
Once you are out of your support network and 24-hour care of a rehabilitation facility, you are largely on your own. You may have helpful and supportive family and friends, but you are the only one who can stop you from drinking again. You must find a way to cope with your feelings and the underlying reasons that you became an addict in the first place. Something has to replace the drinking and now is the time to find your healthy alternatives. Here are some ideas to get you inspired:
- Exercise. Now is a great time to get fit. Find a fun way to be more active, such as taking classes at a gym or learning how to dance. If you enjoy socializing with others, consider joining a league for soccer, baseball, basketball, or any other team sport. The more active you are, the less time you will have to think about drinking. Additionally, exercise and physical movement release natural feel-good chemicals in your brain, so you can literally get a natural high from working out. If you get bored easily, or if working out begins to feel like a chore, change it up and try different things.
- Get creative. Exercise an
 d physical fitness are great for keeping your body fit and for keeping your mind clear, but mental fitness is also important. Stoke your creative fires and tame your urges to relapse. Engaging in something creative is a great way to express yourself and to release the tension that you feel when you have an urge to drink. Try painting, drawing, or even writing. Expressing your thoughts on paper, even if you are the only one who will ever read it, can be very therapeutic. If art has never been your strong suit, consider taking a class at your local community college or community center.
d physical fitness are great for keeping your body fit and for keeping your mind clear, but mental fitness is also important. Stoke your creative fires and tame your urges to relapse. Engaging in something creative is a great way to express yourself and to release the tension that you feel when you have an urge to drink. Try painting, drawing, or even writing. Expressing your thoughts on paper, even if you are the only one who will ever read it, can be very therapeutic. If art has never been your strong suit, consider taking a class at your local community college or community center. - Learn something new. In addition to the creative arts, your mind can benefit from learning something more academic. This could be practical. For instance, you might want to enroll in a local community college and work toward a degree. You can also learn something new just for fun. Maybe you have always wanted to go to Paris. Start learning French so you can go one day and speak with the locals.
- Focus on work. If you enjoy your job, dive in head first and take on new and more challenging projects. If you are not so satisfied at work, this could be a great time to work toward something new and better. Maybe a promotion at your current location is possible. If so, talk to your boss about what you need to do to earn that raise and new position and then put all your energies into doing it. You might also consider searching for and getting your dream job. This is a great way to focus your urges on something positive.
- Pick up a hobby. Maybe you used to work on model trains or you gardened, but your drinking got in the way. Now is the perfect time to get back into your old hobbies. They made you feel good in the past, so use them now as a way to resist the urge to drink. If things from the past hold too many negative memories, start up a new hobby.
- Spend time with family and friends. This may be the most important tool you have in your kit for releasing pressure and avoiding a relapse. When you feel bad, turn to a trusted confidant and vent. Take him out for a cup of coffee and have a good, long, healing talk. Surround yourself with friends and members of your family who are positive influences. A strong social life is key to staying sober and healthy.
Whatever you do to relieve tension and pressure, make sure it is not a return to the bottle. Having come this far, you know you have the strength to stay clean. Use these ideas to help you vent your frustrations and to find an outlet for your excess energy.
Sizzurp is a common slang term for a recreational drug concoction based on promethazine/codeine syrup, a prescription medication used to control coughs and other symptoms related to allergies, colds, and certain additional upper respiratory ailments. In early 2013, this concoction gained new prominence in the media through its connection with a popular hip-hop performer named Lil’ Wayne, who suffered a series of seizures believed to be directly related to his sizzurp intake. In addition to seizures, use of sizzurp can potentially trigger the onset of neuroleptic malignant syndrome, a sometimes fatal condition linked to the intake of the medication promethazine.
 Sizzurp Basics
Sizzurp Basics
Sizzurp qualifies as a recreational drug of abuse because it contains codeine, an opioid narcotic that can produce addiction through repeated use by altering the way the brain creates and uses dopamine, a neurotransmitting chemical responsible for triggering a profound form of pleasure called euphoria. Although specific formulas for making the concoction vary, most batches of sizzurp are based on promethazine/codeine syrup, which contains roughly 6 parts of promethazine for every 10 parts of codeine; the syrup also contains a small amount of alcohol. Other common ingredients in a sizzurp mixture include clear sodas, clear types of alcohol, and melted candies or some other additional source of sugar. People who drink sizzurp often display a characteristic loss of body balance and associated walking difficulties. Apart from these balance changes and euphoria, effects of the concoction typically include a sleep-promoting state called sedation and impairment of the brain’s higher mental faculties.
Promethazine Basics
Promethazine (known more formally as promethazine hydrochloride) is an antihistamine; this means that it counters the effects of histamine, a naturally occurring substance in the body that triggers sneezing, a runny nose, and other symptoms that commonly appear in people who have certain types of allergies. Chemically speaking, promethazine is also classified as a phenothiazine and a neuroleptic. The term phenothiazine describes a variety of substances that act as antihistamines or antipsychotic drugs when they enter the human body. Doctors and scientists sometimes use neuroleptic as an alternative term for any antipsychotic drug.
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome (NMS) is a rare but very serious medical condition that occurs when the effects of promethazine or some other neuroleptic or antipsychotic medication make certain unwanted changes in the normal function of the central nervous system (brain and spinal cord). Although no one knows for sure what causes these changes, one likely candidate appears to be alteration of the brain’s ability to properly process dopamine, the same neurotransmitting chemical linked to the onset of codeine addiction (as well as addiction to almost all other well-known substances of abuse). This connection to NMS is possible because dopamine has other important functions inside the brain, including assisting in the regulation of normal body temperature and regulation of the basic ability to control muscle movement. When dopamine levels change, they can produce profound alterations in these functions.
The National Institute of Neurological Disorders and Stroke lists potential symptoms of NMS that include abnormal muscle rigidity, dangerously elevated body temperature (known medically as hyperthermia or hyperpyrexia), and reduced or altered mental awareness. NMS can also produce significant changes in the normal function of the autonomic nervous system, an involuntary nerve network that helps control ongoing function in the body’s vital organs. Specific changes in this system associated with the effects of NMS can include a rapid heartbeat (tachycardia), unusually rapid breathing, an unstable pulse, unstable blood pressure, abnormally high sweat output, and a form of heartbeat irregularity known variously as an arrhythmia or a dysrhythmia. Ultimately, the effects of neuroleptic malignant syndrome can escalate to a point where they become deadly.
Considerations in Sizzurp Users
Normally, doctors control the risks for neuroleptic malignant syndrome in promethazine/codeine syrup users by limiting the prescribed intake of the medication and screening their patients for the presence of underlying factors that can contribute to the development of the disorder. However, since sizzurp users take promethazine/codeine outside of the context of medical treatment, they don’t receive the benefits of a doctor’s guidance. This makes it likely that very few people who use sizzurp have ever heard of NMS, or have any understanding of the risks they’re taking by using promethazine without a prescription or a physician’s input. It also means that affected individuals may fail to recognize the initial effects of NMS, and therefore may fail to seek help for their condition until serious or severe health complications arise. Since sizzurp use is fairly new from a medical research standpoint, no one really knows how many people are at risk for the unexpected onset of NMS.
If you knew something was a risk for cancer would you avoid it? Known carcinogens are usually highly publicized and people frequently adjust their behavior accordingly. One thinks of red dye #2 that was once added to bacon. Sun block sales suggest that many take the risk of skin cancer from sun exposure seriously. And the current intolerance for tobacco use is at least partly driven by the public’s knowledge that smoking causes cancer. Yet, how many are aware that alcohol is also a dangerous carcinogen?

Alcohol is a clear cancer risk, but it gets little public attention as such. According to the World Health Organization, alcohol is responsible for 4 percent of the world’s cancers and is the third greatest risk for developing a host of other serious diseases as well. In the United States, a study published in mid-February in the American Journal of Public Health, states that alcohol is responsible for approximately 20,000 cancer deaths each year–equivalent to about 3.5 percent of all U.S. cancer deaths, according to a news release from the Boston University Medical Center. That translates to 20,000 cancer deaths connected to alcohol consumption. Certainly, alcohol as a cancer risk deserves a bit more press.
In the first major analysis of alcohol and cancer in recent decades, the study looked at 220,000 U.S. adults and examined their alcohol use and mortality information. The researchers found that seven cancers appeared to be particularly linked to alcohol use. Those cancers were: rectal, colon, liver, esophageal, breast (female), pharynx, larynx and oral cancer.
As many as 15 percent of women’s breast cancers were connected to drinking alcohol, a finding which is backed up by the Journal of the American Medical Association (JAMA). This is probably because alcohol affects estrogen levels. In men, cancers linked to alcohol use were oral, larynx, pharynx and esophageal. The data showed that men and women who consumed three or more drinks each day increased their cancer risk by 48 to 60 percent. One-third of cancer deaths were linked to just one to two drinks per day.
The leading risks for cancer are a person’s weight, diet, activity level, tobacco and alcohol consumption. While some have touted drinking certain kinds of alcohol as beneficial to heart health, the facts show that alcohol leads to 10 times more fatalities than it prevents. In fact, those who contract cancer related to alcohol use lose an average of 18 years from their lives.
“The relationship between alcohol and cancer is strong, but is not widely appreciated by the public and remains under-emphasized even by physicians,” said Timothy Naimi, who served as the paper’s senior author. “Alcohol is a big preventable cancer risk factor that has been hiding in plain sight.”
04 Apr 2013
Long Term Effects of OxyContin on the Brain
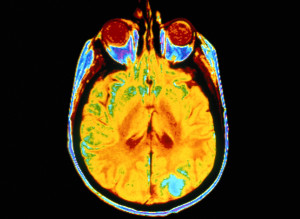
 Most drugs of abuse ultimately have an impact on the brain. The levels of the different neurotransmitters (the brain’s chemical messengers) are carefully balanced, so the brain can apply a reward chemical when a reward is in order and a painkiller when one is required. Drugs of abuse tend to subvert these normal processes, often releasing an excessive amount of the brain’s reward chemical. Finding out about the specific risks for one of the most commonly abused prescription drugs, OxyContin, helps you understand how addiction develops and the long-term risks of the drug.
Most drugs of abuse ultimately have an impact on the brain. The levels of the different neurotransmitters (the brain’s chemical messengers) are carefully balanced, so the brain can apply a reward chemical when a reward is in order and a painkiller when one is required. Drugs of abuse tend to subvert these normal processes, often releasing an excessive amount of the brain’s reward chemical. Finding out about the specific risks for one of the most commonly abused prescription drugs, OxyContin, helps you understand how addiction develops and the long-term risks of the drug.
What is OxyContin?
The simplest way to understand OxyContin is as an opioid drug like heroin or opium. It is derived from the same source, and has the same basic effects as these illicit substances. Opioids are widely used in medicine because they are among the most efficient pain relievers. Many people come into contact with drugs such as Vicodin, Percocet and OxyContin through legitimate means. The main defining feature of OxyContin is that it has a time-release formula, the effects lasting for about 12 hours. Percocet releases all of the substance at once and lasts only about five hours.
What are the Effects of OxyContin?
OxyContin works through its interaction with the opiate receptors in the brain. By binding to these receptors, the drug reduces feelings of pain and triggers the release of dopamine, the most important neurotransmitter in the brain’s reward system. This creates a mixture of euphoria and pain relief, bringing about a relaxed and contented mood in the user. It also depresses the central nervous system, which is responsible for many critical processes within the body, including heart rate, digestion, pain messages and breathing. Although the time-release formula makes it more difficult to achieve the euphoric high most users are looking for, many chew the drug or even inject it for a bigger rush. They will also take more than is suggested by their doctor to increase the effect.
 The Long-Term Effects of OxyContin on the Brain
The Long-Term Effects of OxyContin on the Brain
Addiction is the most evident effect of long-term OxyContin abuse on the brain. The brain is initially overwhelmed when the drug signals the extended release of dopamine, unable to continue its normal functioning because of the intense chemical injection. To account for this, as the drug is taken more regularly, the brain adjusts its natural processes so it isn’t overwhelmed anymore. By reducing the number of opiate receptors and producing less dopamine naturally, the brain effectively dampens the effect OxyContin has. This means that the user has to take more of the drug to achieve the same effect, and that without the drug, he or she will have a deficit in some neurotransmitters.
This effect creates addiction, because the brain has essentially rewired itself to account for the continued presence of the particular substance. Without it, the individual experiences a wide range of unpleasant side effects, known as withdrawal. The longer the individual takes the drug and the more that is consumed, the more the brain adapts and the individual becomes addicted. Although using OxyContin more than prescribed commonly leads to addiction, it can also develop from the suggested course of medication.
Many of the long-term effects of the drug come to the forefront during this withdrawal period. Withdrawal usually creates the opposite effect of the drug, so if a woman goes without OxyContin for the first time after months of abuse, she will experience severe pain, depression and flu-like symptoms such as loss of appetite, runny nose and sneezing. Irritability and mood swings are also common. Because of these effects, the cravings for another dose of the drug can be intense.
One of the main risks of any opioid drug is respiratory depression (or slowed breathing). This is because the drugs depress the central nervous system, which is responsible for breathing. The risk of this is greater in long-term users, those who take more of the drug than prescribed, and anybody who combines it with alcohol.
Finally, there is a risk of severe psychological disturbances in people who abuse OxyContin. In long-term users, hallucinations, delusions, and delirium have all been reported, in addition to mood swings and panic attacks. This doesn’t occur in all cases, but is often worse during withdrawal, when many users feel confused or disoriented. Memory issues or even amnesia can develop in long-term abusers.
Need for Psychological Support
Addiction is the major long-term effect of OxyContin use because it drives the individual to keep abusing the drug and thereby makes all of the other potential consequences more likely. Being able to recognize the signs of addiction is extremely useful, but the best way to minimize your risk is to take the drug as advised by your doctor. If addiction does occur, psychological support can help you overcome your issues and therefore reduce the risk of other ill-effects.
The blood-brain barrier (BBB) is a network of tiny blood vessels (capillaries) that separates the interior of the central nervous system (brain and spinal cord) from the rest of the body’s circulatory system. This separation is required to help the brain maintain a stable internal environment and function properly; it also helps protect the brain from infectious microorganisms. Cocaine and methamphetamine can significantly damage normal function in the blood-brain barrier; in turn, this damage can open up the brain to infection and other processes that can produce severe or life-threatening changes in brain health.
Blood-Brain Barrier Basics
Capillaries are the body’s smallest blood vessels. They sit at the junction between the arteries—which carry oxygen-bearing blood to various organs and tissues—and the veins, which carry oxygen-depleted blood and carbon dioxide waste from the organs and tissues to the heart (on the way to their eventual destination point in the lungs). It’s inside the capillaries where exchange of the oxygen and carbon dioxide content in the blood occurs.
In every location except the blood-brain barrier, the capillaries have relatively large openings in their walls that allow large and small molecules to move in and out of the bloodstream. This level of access means that any required substance produced in most of the body can easily travel through the bloodstream and get where it needs to go. However, it also means that conditions in the tissues fed by the capillaries can change rapidly and relatively chaotically as different molecules move in and out of circulation.
The central nervous system in general (and the brain in particular) can’t handle the sorts of fluctuations that occur when all molecules can flow easily through the capillary walls. In fact, these fluctuations would destabilize the brain to the point where it wouldn’t be able to perform its function as the body’s command and control center. In addition, if any molecule could easily enter the central nervous system, then infectious microorganisms could get to the brain and wreak all sorts of havoc on the organ’s structures and activities. In order to help prevent these possibilities, the capillaries in the BBB are very tightly constructed and lack the large openings found in other capillaries. In addition, supporting cells (called astrocytes) sit in the barrier outside the capillary walls and further block any influx of unwanted molecules and microorganisms.
The Effects of Cocaine and Methamphetamine
For a number of reasons having to do with how cell walls are constructed, molecules that dissolve easily in the presence of fat can pass directly through the capillary walls in the blood-brain barrier. Among the molecules that can access the central nervous system in this way are cocaine and methamphetamine. Once inside the central nervous system, these drugs produce mind alteration and a variety of other effects by altering the normal levels of certain neurotransmitting chemicals—such as dopamine, norepinephrine and serotonin—that support proper brain function by passing on required messages between millions of nervous system cells called neurons.
 One of the consequences of neurotransmitter alteration by cocaine and methamphetamine is a significant increase in the amount of heat retained inside the brain and body. If heat levels get too high, they can trigger a condition called hyperthermia, which literally means “overheat.” In turn, hyperthermia can produce serious damage in the capillary walls inside the blood-brain barrier and lead to the formation of significant gaps that give access to dangerous molecules not usually allowed into the central nervous system’s restricted environment.
One of the consequences of neurotransmitter alteration by cocaine and methamphetamine is a significant increase in the amount of heat retained inside the brain and body. If heat levels get too high, they can trigger a condition called hyperthermia, which literally means “overheat.” In turn, hyperthermia can produce serious damage in the capillary walls inside the blood-brain barrier and lead to the formation of significant gaps that give access to dangerous molecules not usually allowed into the central nervous system’s restricted environment.
Apart from its role in hyperthermia, cocaine produces chemical changes in the capillary walls that lead to the formation of abnormally large points of entry through the BBB, according to a study published in 2010 in Blood, the journal of the American Society of Hematology. These chemical effects are particularly prominent in cocaine users who have HIV infections, and the authors of the study believe that the relatively rapid advancement of HIV’s brain effects in cocaine users stems from the ability of both cocaine and HIV to damage the capillary structures in the blood-brain barrier. Cocaine may also damage the BBB by increasing the flow of blood plasma to the brain, or by encouraging an excessive flow of the neurotransmitter serotonin from the body to the brain. In addition to its role in hyperthermia, methamphetamine can apparently damage the blood-brain barrier through a direct, toxic effect on the capillaries within the barrier.
Doctors and researchers have long looked for a medication capable of easing the effects of cocaine addiction. For a variety of reasons, their past efforts haven’t been successful, and there is no single medication on the market capable of filling this role. However, current evidence indicates that two other medications-buprenorphine and naltrexone-that were initially designed for other purposes, apparently work in combination to ease cocaine addiction and facilitate successful participation in cocaine rehab programs. Doctors usually use buprenorphine to treat opioid addiction, while naltrexone is used to treat both opioid and alcohol addiction.
Read More
Methamphetamine is known for its ability to damage normal brain function in its users. Unfortunately, some of the damage done by the drug increases the likelihood that recovering addicts will experience a relapse and return to active methamphetamine abuse. At one time, doctors and researchers believed that meth addicts were incapable of regaining the mental function required to significantly decrease any relapse risks. However, current evidence indicates that many of the brain deficits that can lead to relapse will gradually fade away if people addicted to the drug can remain in recovery for an initial, crucial period of time.
Read More
Substituted amphetamines are a group of chemically related substances that possess a strong chemical resemblance to the manmade stimulant drug amphetamine. Some of these substances-including ephedrine, pseudoephedrine, and cathinone-come from plant sources and predate synthetic amphetamine by thousands of years or more. Others-including methamphetamine and MDMA (Ecstasy)-are synthetic and have only existed for anywhere from decades up to slightly more than a century. Almost all substituted amphetamines produce pleasure and stimulant effects in the central nervous system; to varying degrees, they may also produce hallucinations and increased feelings of connectedness toward others. Side effects common to most of these substances include potentially deadly toxic reactions (overdoses) and long-term risks for drug addiction.


