The misuse of prescription drugs has become a serious problem in the United States. In many situations a prescription is written for a legitimate health problem, it’s used for a time and then left forgotten in a medicine cabinet.
Teens raid their parents’ and other relatives’ medicine cabinets to pilfer prescription drugs and the drugs are taken to parties where they’re mixed in combination with various other drugs. This practice can be dangerous, even deadly.
 While pain medications are a common choice, another drug readily available is Adderall, which is prescribed for attention deficit hyperactivity disorder (ADHD). This stimulant can allow students to focus and avoid sleep for days in an effort to work on a task or study. However, there are dangerous side effects, including heart palpitations and painful urination.
While pain medications are a common choice, another drug readily available is Adderall, which is prescribed for attention deficit hyperactivity disorder (ADHD). This stimulant can allow students to focus and avoid sleep for days in an effort to work on a task or study. However, there are dangerous side effects, including heart palpitations and painful urination.
The Study
Along with improved academic performance, Adderall can also improve athletic performance. A recent study published in the Journal of Studies on Alcohol and Drugs provides an analysis of Adderall use among adolescent athletes.
The researchers accessed data from the Monitoring the Future survey that gathered information from 8th and 10th graders in 2010 and 2011. The survey included 21,137 teens and measured the past-year non-medical use of the drug and used logistic regression analysis to determine if there was a connection between the level of involvement in competitive sports and nonmedical Adderall use.
The results showed that Adderall use was more pervasive in certain sports and there were differences between the genders. Males that played lacrosse and males that wrestled were more likely to use the drug, while females did not show any patterns of use based on particular sports.
The Findings
The study’s findings showed that certain sports, particularly those involving a high level of contact, may lead to pressure among males to improve performance through a stimulant like Adderall.
How Parent’s Can Help
Parents may not realize the stress that their children deal with as they compete for grades and placement on sports teams. In many cases, the teen may feel that parental expectations are adding to their stress, so a parents’ reassurance may help them avoid the danger of drug use.
Parents can help their children avoid the misuse of Adderall and other prescription drugs by talking regularly about the pressures of school and extracurricular activities, including sports. They can also work to maintain some level of contact with teachers and coaches to help ensure that their teen is exhibiting healthy behaviors related to school, sports and extracurricular activities.
Click Here – To Read More About Teen Substance Abuse
10 Sep 2013
Huffing: A Dangerous Trend For Teens
Alcohol, street drugs, prescription drugs and over-the-counter medications are not the only way kids are getting high and it is imperative that parents become aware. Teens are “huffing” all sorts of common household items in order to get a fast buzz.
 Teens and preteens looking for a cheap high are willing to experiment with breathing in powerful household products like nail polish remover, hair spray, aerosol deodorants, computer cleaner, correction fluid and even aerosol from whip cream canisters. These and other toxic substances are found in nearly every room in American homes. The problem is that many parents, like their young teens, fail to recognize the dangers. A single attempt at huffing has been enough to kill some youth.
Teens and preteens looking for a cheap high are willing to experiment with breathing in powerful household products like nail polish remover, hair spray, aerosol deodorants, computer cleaner, correction fluid and even aerosol from whip cream canisters. These and other toxic substances are found in nearly every room in American homes. The problem is that many parents, like their young teens, fail to recognize the dangers. A single attempt at huffing has been enough to kill some youth.
Huffing is also called dusting or sniffing. Kids trap the toxic chemicals in a small plastic bag which they then hold up to their face before inhaling deeply. This gives them a five to 10 second rush or high. Teens inhale magic markers, household paint, Freon from air-conditioners and refill cartridges for butane lighters.
Dangerously False “Safer” Perception
In recent years there has been a trend among teens away from illegal street drugs towards substances that teens consider more ‘safe.’ Prescription and over-the-counter medications became more widely used for a time until cost and safety measures made them hard to come by. Now inhalants are popular. Not only do these products seem harmless to teens, they are also inexpensive and easy to obtain. Most of the time teens can simply help themselves to something already on the shelf at home. If not, no one will question them when they buy these things at the store.
The truth is that these products are safe when used for their intended purposes and according to their package directions. They are anything but safe when inhaled in order to get high. At best, repeated exposure will injure vital organs (kidneys, liver, lungs, heart and brain). At worst, kids can experience heart attack – referred to as Sudden Sniffing Death Syndrome – or suffocation. Parents who had no idea their child was huffing have gone into their child’s room to find them dead on the floor with a bottle of computer cleaner still clenched in their fingers.
Parents should talk with their teens and even preteens about the dangers of breathing in toxic fumes and chemicals. Kids are huffing even in elementary school, so it isn’t a discussion that needs to wait for high school – it can happen while using these household items or it can be part of a sit-down conversation about drug use in general. Tell your kids that while a product can be safe to use it can still be poisonous. Poison is an important adjective since it communicates just how serious these substances really are.
Parents Can Also Keep Their Eyes Open To Signs Of Huffing, Including:
- Finding plastic bags with a chemical odor to them
- Aerosol products or strong chemical items disappearing entirely or running out quickly
- Teens having the smell of chemicals on their breath
- Symptoms of intoxication, such as red and watery eyes, slurred speech or dazed appearances
- Paint, correction fluid or magic marker stains on their face
- Household products being out of place or perhaps even in the teen’s room.
The best defense is a strong offense, so talk with kids about what their friends might be doing. Talk about why kids might be looking to get high. If your child is huffing regularly, get professional help. Huffing can be addictive in the same way as drugs or alcohol, and kids won’t know which sniff could be their last.
03 Sep 2013
Fentanyl “Patches” – Deadly For Children
A 12-year-old girl from Clinton, Missouri was found dead in June 2013 after a suspected overdose of the Fentanyl patch. Destiny Spilter died after she stuck a used fentanyl patch on her thigh. The patch had been previously worn by her grandmother who, once done with it, threw it in the trash.
Fentanyl is an extremely strong opioid used to manage pain. It is 100 times more potent than morphine and 40 times stronger than heroin. Overdoses, some even fatal, are common.
Many patients are prescribed Fentanyl when other types of narcotic pain medications no longer offer relief. In most cases, this is because the body has developed tolerance to the pain killer, and it needs more and more of the substance to offer the same type of relief. Since many medications are lethal at such high doses, doctors must look to a different medication altogether instead of just increasing the dose of the current prescription. Fentanyl is a favored tool in the pain-management arsenal.
Use with Extreme Caution
Despite its benefits, however, Fentanyl must be used with extreme caution as even patients who have topped out of their traditional pain medications have found it to be too strong to tolerate. The patch, even at its lowest dose, has the potential to reduce respiration to the point of death.
The Fentanyl patch was created to offer continuous relief to patients in chronic pain, but over a period of several days. If a person were to ingest that amount of Fentanyl all at once, it would likely be fatal. Given its high potency, there are a number of safety advisories and side effect warnings regarding use of the drug. One of the FDA warnings recommends flushing the patch after use so that unintended recipients do not ingest the remaining residue — either accidentally or on purpose. Even though the Agency recognized that there may be some environmental concerns about flushing, it felt that the risk associated with accidental exposure far outweighed any potential risk to the environment or water sources.
Tragedy – Too Often
Destiny’s grandmother, who was using the patch to manage her chronic back pain, did not follow these fairly simple instructions. Not surprisingly, the curious young girl found the patch and put it on, perhaps mimicking the behavior she previously observed in her grandmother. Even after the patch is used for three days, studies show that it could still contain more than 50 percent of the original Fentanyl dose. Her body was unable to handle even the amount of Fentanyl that remained in the patch and she died.
Unfortunately, accidental overdose is not uncommon for the Fentanyl patch — especially in children. Children may be initially attracted to the patch, thinking that it is a sticker. And because the patch is meant to stay on the skin for up to 3 days, there is typically plenty of glue remaining to keep it securely on the child’s skin. If they place it in an area that is hidden by clothing, caretakers may not notice it until the damage has been done.
19 Jul 2013
Without Screening Alcohol Abuse May be Missed
Patients come into a doctor’s office and give their symptoms to the doctor. The doctor listens, nods his head, and starts to piece together the symptoms the patient is mentioning and what he thinks may be the cause of those symptoms. But sometimes the patient doesn’t share everything with the doctor and the doctor does not ask some questions that could determine the causes or aggravations of an illness.
A new study from the School of Medicine at The University of Texas Health Science Center in San Antonio reveals that some questions doctors may not be asking are related to alcohol consumption. The article, in the Annals of Family Medicine, states that doctors may miss alcoholic symptoms in three out of four patients who come into their office.
 Screening Can Provide Proper Treatment
Screening Can Provide Proper Treatment
Researchers at UT Medicine conducted a study to see how well physicians could identify patients that exhibited symptoms of alcohol abuse. Over 1,600 participants were gathered from 40 primary care practices across multiple central states.
After participants were asked questions about their drinking habits, doctors were asked to make a diagnosis of whether or not the person was at risk for alcohol abuse. Participants were asked about the frequency that they drank alcohol and whether or not their drinking caused them to be reckless to themselves or with others. Doctors then categorized them in different alcohol use groups, including non-harmful drinker or harmful drinker.
Study co-author, Dr. Barbara Turner, stated that a doctor’s hunch missed identifying three out of four participants at risk for alcohol abuse. When doctors did suspect a person might be abusing alcohol though, the doctor was usually right.
Excessive Alcohol Consumption Hurts in Many Ways
Study authors believe that if patients were screened for their drinking habits that doctors may be able to help treat much more than alcoholism. High blood pressure, diabetes, liver disease, and some cancers have been connected to excessive drinking of alcohol. The 2011 National Health Interview Survey stated that over 85,000 people die each year from a circumstance where alcohol was misused.
Earlier studies reveal that when doctors have been able to identify harmful alcohol consumption habits in their patients, their patients decreased their alcohol consumption and improved their lives. Doctors provided brief counseling sessions to help their patients succeed in alcohol reduction.
Changing Procedures
Doctors can only treat what they see that needs to be treated. A screening procedure to help them identify a patient’s possible problems with alcohol use may help them better fully treat their patient.
Dr. Turner suggests that doctors screen their patients regularly to identify any changes in their drinking habits. A person may start drinking more heavily after both good and bad times like the following:
- Divorce
- Death of a loved one
- Loss of a job
- A new job or promotion to be social with new colleagues
- Celebrating with friends
If doctors catch harmful drinking patterns early, they may help prevent risky actions and future health problems in their patients.
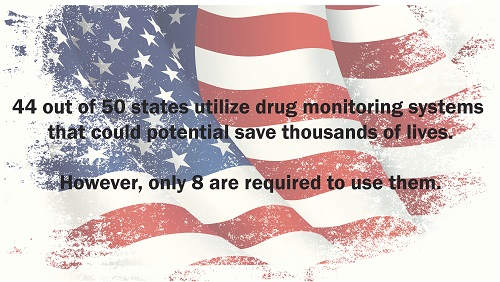
Many state legislatures have enacted laws to make it easier for them to establish a prescription database to track drug abuse. These programs are often put in place to assist law enforcement in cracking down on illegal activity such as producing methamphetamine. Clandestine laboratories rely on large amounts of cold medicine to produce their dangerous substances that wreck lives. Most of that activity has been squelched by drug monitoring programs; another advantage to these programs affects more than just law enforcement.
The monitoring programs also help point the way to users who are likely abusing a prescription drug, which can lead interventions that are potentially life saving. These programs, which are now up and running in 44 states, have proven to be an invaluable tool for healthcare providers. They are now able to legally monitor the frequency of prescription drug use among their patients. The drugs being monitored include opioids, amphetamines and sedatives. But laws vary per state and only eight states currently require providers to participate in the monitoring programs.
What is certain is that the states that do allow a monitoring program have less of a problem with the current epidemic of pain killer abuse in this country. While not much is known about how the monitoring programs are affecting the way doctors prescribe their drugs, one study done in Ohio shows that more than 40 percent of emergency room doctors who had access to their patient’s prescription drug history made different prescription decisions based on the data from the monitoring program.
Almost all physicians are pressed for time, which means their ability to thoroughly study the data available to them is hampered. Furthermore, the amount of resources available to healthcare professionals to fully interpret the data providing by monitoring programs is also in short supply, limiting the impact that the data could have on the health of patients across the nation.
11 Jul 2013
Relapse Prevention: Study May Have Found Key to Preventing Stress From Triggering Relapse
For the person who has fought back against drug addiction and has been walking the road of recovery, stress can pose a dangerous threat. For many, the stress of struggling to find work, rebuild relationships, or a sudden loss through death can be enough to trigger a return to using drugs. Stress is a powerful force for people without an addiction history, but when there has been a pattern of soothing stress with substances, the temptation to do so again when the stress temperature rises is great. A recent National Institutes of Health-funded study may have discovered the key to preventing stress from triggering that kind of relapse.
The grant-funded study was actually a partnership between researchers from the University of Pennsylvania and Brown University. The investigation provides a clear outline for the sequence of events within the brain leading up to a stress-induced drug relapse. The study debunked prior hypotheses about the relapse pathway and uncovered evidence that the part of the brain connected to meeting basic needs (the VTA) was pivotally involved.
The study employed rats with a history of cocaine addiction but who were not presently addicted. Some of the rats were treated with a chemical (nor-BNI) that inhibits certain VTA receptors (known as kappa opioid receptors), while the other group of rats did not receive the treatment. Next, all of the rats were made to undergo five minutes of stress-inducing exercise. Observation showed that the treated rats did not revert to cocaine use even after being stressed. The non-treated rats did go back to cocaine.
When we meet our body’s essential needs such as eating and drinking, the brain releases dopamine, a chemical that rewards our behavior with a sense of pleasure. At the same time, healthy brains also release GABA, which modulates dopamine release. Drugs keep GABA from doing their job of controlling the dopamine flow and hence drug use produces an oversized rush of good feelings.

Relapse Prevention with Stress Prevention
In this study, researchers first demonstrated that stressors prevent GABA from slowing down dopamine release. This explains how stress can be a preamble to drug relapse. In the presence of stress, the proper amounts of reward chemicals are disordered. Pleasurable activities become inordinately pleasurable. However, the study team showed that by introducing nor-BNI into the VTA area of the brain, the dopamine controls remained in place even during periods of stress.
By honing-in on the neural underpinnings of a stress-caused relapse, these scientists may have found a way to interrupt the chain reactions that trigger a return to drug use. The study could prove to be a major leap forward toward creating a targeted medication that could remove a domino from the stack and prevent the inevitable result.
Finding a rehab that has not only a great rehabilitation program but a great aftercare program is another way to help prevent relapse. Read Choosing the Right Drug Rehab for Your Loved One to learn more.
The problem of inhalant abuse has surfaced again in a recent story from California, where nitrous oxide abuse is linked to the death of a college student. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), over 1 million Americans abuse inhalants each year, and they’re keen to point out that the problem is far from confined to adolescents. In the wake of the incident, law-makers in California are looking at implementing new legislation and raising awareness to reduce the numbers of needless deaths from inhalant abuse. However, the strategy appears to be geared toward young people, when national research has shown that the majority of inhalant admissions are actually from adults.
The Recent Death
Nineteen-year-old Claremont McKenna College student Ali Mirza was found with nitrous oxide canisters, or “whippets,” in his dorm room when he died. He was rushed to Pomona Valley Hospital Medical Centre, after paramedics failed to revive him at the scene of the incident last month. He was pronounced dead at 2am on May 17th, and his funeral is scheduled for the June 15th. His family and friends will mourn his untimely passing, but the increased efforts of police officers and law officials to combat inhalant abuse may prove to have positive consequences for LA’s youth.
The Dangers of Inhalants
“Inhalants” is actually a fairly broad term to describe drugs that are “huffed” by users and many different substances could fall under the group. These include paint, marker pens, glue, air freshener, butane and substances like nitrous oxide. Despite the large number of substances used, most of them have similar effects to anesthetics and carry numerous potential risks. The most widespread (being a possibility with all inhalants) is sudden sniffing death syndrome, which basically results from a disturbance to the heart’s natural rhythm and is often fatal. Inhalants can also cause brain cell death, lung damage, short-term memory loss, and liver and kidney damage.
Nitrous oxide balloons (commonly known as “laughing gas”), in particular, pose a problem because the effect of a single “high” only lasts for five minutes or less. This means that users will generally repeat doses in a single evening of use, and this multiplies the potential for damage. When the user is “huffing,” he is depriving himself of oxygen, and repeated oxygen deprivation can lead to unconsciousness or—over time—brain damage.
The Response
The problem of inhalant abuse has been on the rise among California youths, according to Veronica De Alba (a deputy city attorney in LA), and this has led her to push for increased legislation to protect California adolescents. Police in the area are working on an ongoing 15-month investigation – entitled “Operation No Laughing Matter” – to curb the usage and availability of nitrous oxide. This has dramatically reduced the supply of the drug in the LA County area, but a continued effort is evidently required to prevent resurgence in usage down the line.
 Not Just Teens
Not Just Teens
Research from SAMHSA has shown that adults actually make up the majority of admissions to treatment facilities for inhalant abuse. The study showed that out of all admissions to treatment facilities for inhalant abuse, 54 percent were from people aged 18 or over in 2008. Admittedly, the majority of these admissions (52 percent) were from those in the 18 to 29 age group, but it still calls the adolescent focus of recent efforts into question.
While there is obviously a problem with inhalant abuse among teens, the problem is far from confined to them, and any public health-focused responses should take this into account. The sad truth is that inhalant abuse, like all drug abuse, may be commonly associated with troublesome youths, but it’s actually common in people from all walks of life. Some similar assumptions, which may be made about the race of inhalant abusers, were also addressed by the study and the results showed that the majority of the admissions were white males.
Broadening the Scope of Prevention and Education
Public awareness of the dangers of huffing will undoubtedly be improved by the recent story, but it’s important that you don’t mentally file it way as something that only really affects young people. The negative health impacts of huffing don’t discriminate based on age—they can affect any user—and research seems to show that adults are actually more likely to be heavy huffers. Broadening the scope of inhalant awareness campaigns to also appeal to adults initially seems like an unnecessary step, but statistics tell us that it’s just as vital as targeting teens and young adults.
There is little argument that America is in the midst of an opioid epidemic, but health officials will argue about how to solve the problem.
Scientific articles published recently in the same journal represent ideas that conflict. The Annals of Internal Medicine, a publication established in 1927 by the American College of Physicians, published two articles on the subject of restriction prescription in hospital emergency departments. The issue revolves around the current guidelines for how much pain medication should be kept in the pharmaceutical areas of emergency departments. One side of the debate says that the current regulation of a three-day supply is not enough for the average emergency department. The other side of the debate says the limited supply will force doctors to make wiser choices in who gets what pain medicine.
Prescription Drug Abuse
New York City made headlines earlier this year when city officials announced that the most powerful and common painkillers on the market today would be restricted in the city’s 11 public hospitals. The move was in response to the abuse of painkillers that has gripped the city. These painkillers include Vicodin, OxyContin and Percocet. Methadone and Fentanyl are no longer distributed in the public hospitals. Those in favor of the restrictions note that there has been a rapid increase in opioid analgesic consequences and that restricting the medications in question will help doctors provide safer care for their patients who are experiencing issues with pain.
Many Americans now have an expectation that a visit to the emergency room will result in acquiring pain medication. Some emergency department personnel agree that something has to be done about that perception, which is bolstered by doctors that could perhaps be less willing to doll out the drugs to patients in pain. Non-narcotic medications are now beginning to find their way into emergency departments, as are pain meds that are engineered to be less addictive.