06 May 2013
The Battle Over Legalizing Marijuana Continues
Marijuana continues to be in the headlines after legalization in Washington and Colorado, Obama’s references to whether or not his administration will pursue those who violate the federal laws against its use and the latest ruling by an appeals court to reject the change in classification for the drug are top news headlines.
Despite efforts by those who believe the drug is safe for medicinal and even recreational use, the DEA believes it still has a high potential for abuse and therefore the classification that it currently has no acceptable medical use stays in place. As a result, marijuana will continue to be treated by the federal government as a drug akin to LSD and heroin.
 While those battling the drug war on the home front appear to be satisfied with the ruling, those who wish to conduct research believe their hands remain tied. According a recent ABC News report, the restrictions meant to protect the people are the very restrictions that make it difficult to perform the necessary studies to convince the DEA that the drug should be moved into a different category.
While those battling the drug war on the home front appear to be satisfied with the ruling, those who wish to conduct research believe their hands remain tied. According a recent ABC News report, the restrictions meant to protect the people are the very restrictions that make it difficult to perform the necessary studies to convince the DEA that the drug should be moved into a different category.
Essentially, the DEA wants FDA approval before removing marijuana from Schedule I classification. The research that the FDA needs completed to be able to provide approval cannot be conducted because of the current laws in place. The argument was made by the Drug Policy Alliance, suggesting that the federal government is responsible for blocking the research that needs to be completed.
While a number of studies have been completed or are underway, the biggest obstacle observed by opponents to the DEA classification is the fact that the studies must have FDA approval before they can begin. This is perceived by many to be a conflict of interest.
Read More About The Pros And Cons Of Legalizing Recreational Marijuana
24 Apr 2013
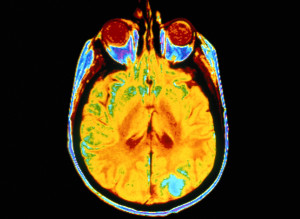
Drug Addiction ‘Turned Off’ With Lasers
A groundbreaking study on rats from the National Institutes of Health may herald a revolutionary new treatment for cocaine addicts. By identifying a specific region of the brain that is diminished in rats susceptible to cocaine addiction, researchers were able to reduce their drug-seeking behavior by targeting the light from a laser onto the specific area. The effect is truly remarkable—by essentially reinvigorating the area in the brain, the drug-seeking behavior was notably reduced. If this is applied effectively to humans, it could provide a unique and effective approach to the treatment of numerous drug addictions.

Modeling Addiction in Rats
Research on rats might not seem like the best model for drug addiction in humans because of the obvious differences between us as species. However, it’s been found that the neural pathways in rats are nearly identical to those in humans, so rats are actually excellent models for addiction. Like humans, some rats display a tendency to become addicted to drugs while others don’t have the same problem. This is tested using a cocaine-dispensing lever, and it was found that some rats compulsively take cocaine while others weren’t particularly interested. The fact that the addicted rats continue to push the lever to get the drug even when it results in an electric shock to the foot further adds weight to the model. This research indicates that there is an underlying physiological reason that some humans become addicted and some do not.
Identifying the Region
The University of California researchers built on existing brain imaging research which identified that deficits in the pre-frontal cortex region were associated with drug addiction by looking at addicted rats. They compared the neuron firing patterns in addicted rats to those of non-addicted rats and confirmed that cocaine produces bigger defects in the addiction-prone animals. The precise targeting of the region enabled them to make specific alterations to see if it affected the animals’ behavior.
Treating the Condition
Making minute alterations to the functioning of specific areas in the brain is obviously challenging and potentially dangerous. By making genetic alterations and introducing light-sensitive compounds into the rats’ neurons, the researchers were able to make the biological equivalent of a switch. They did this in the brains of both the addicted and non-addicted rats so they were able to test the theory in two ways. Shining a laser light at the compound flicks the switch, activating or deactivating the specific region of the brain and therefore either creating or removing the defects seen in drug addicts.
The results confirmed the theory. When the “switch” was activated in the addicted rats—removing their inherent deficits—they didn’t press the lever as often for a dose of cocaine. Astoundingly, when the switch was deactivated in the non-addicted rats (mimicking the addicted brain) they actively used cocaine more. This is particularly important because it establishes a causal link between this defect and addictive behavior.
Applying it to Humans
Thanks to the similarity between human and rat brains, the research can be easily applied to humans, and clinical trials are already in the planning stages. However, lasers will probably not be used in the human version of the treatment, according to the researchers, with the preferred method being trans-cranial magnetic stimulation. This basically uses an electromagnet placed outside the scalp to achieve the same effect. The treatment is currently used for the treatment of depression, and could be easily adapted for the new purpose.
What Does It Mean for Treatment?
Cocaine addiction is one of the most challenging addictions to treat from a medical perspective, because there aren’t any FDA-approved medications which can be used for it. If this approach is shown to be successful in clinical trials, it could provide a valuable tool for rehabilitation centers all across the country. Medical treatments can’t fully address the multi-faceted issue of drug addiction, but by reducing cravings it allows counselors and other psychiatric professionals to deal with the underlying psychological issues that lead to addiction.
Although the initial research focused on cocaine addiction, the treatment could also be applied to other drugs. Different chemicals have different effects, but psychoactive drugs can be broadly classified as working through a similarity to natural compounds, often the “reward” chemical dopamine. This means that there is a great degree of similarity between different addictions (even when substances are not involved) and that making small modifications could allow the treatment approach to work with other drugs.
It is not a “magic bullet,” however. Drug addiction often results from things like poor methods of dealing with problems like stress or depression, and correcting the neurological differences doesn’t teach substance abusers better coping mechanisms. The non-invasive nature of the treatment is extremely promising, but it won’t “cure” the problem in the same way that drugs for opiate addictions haven’t stopped heroin abuse. However, the new research may provide a valuable component to a multi-faceted approach to treating drug addiction.
17 Apr 2013
‘Huffing’ a Growing Problem in Adults
Huffing. Sniffing. Bagging. No matter what it’s called, inhalant abuse is an ongoing problem in the adolescent population. Unfortunately, increasing evidence shows that adults are latching onto this dangerous form of substance abuse as well. If you suspect an adult you love is abusing inhalants, it’s critical to learn more about this dangerous habit and get him or her into drug rehab treatment.
Adults now make up more than half of the patients being admitted to treatment for inhalant abuse, according to a survey by the Substance Abuse and Mental Health Services Administration. It’s not just young adults either. The survey revealed that 32% of the admitted adults were between the ages of 32 and 44 while 16% were older than 45. Overall, an estimated 1.1 million adults abused inhalants in the last year .
Inhalants are attractive to drug users for several reasons. Because the chemicals are found in household products, they’re easy to find. There’s no need to visit a shady part of town to buy them. Inhalants are also inexpensive, making them an accessible substance for people of any economic status.
Inhalants are Toxic Chemicals
While all abused substances carry potential risks, inhalants are particularly dangerous. Inhalants are breathable chemicals found in many everyday products, from furniture polish to computer cleaner sprays. Other commonly available inhalants include whipped cream aerosol cans, vegetable oil sprays, varnish removers, paint thinners, correction fluids, and felt tip markers. When used as intended, we don’t feel the effects of the chemicals inside the products.
However, when the products are abused, they create a high. Inhalants are usually taken directly into the lungs by breathing in the chemical through the nose or mouth directly from the container or from a bag filled with the chemical. Some users will inhale directly from a cloth soaked in the chemical. The high produces hallucinations and feelings of euphoria. Addicts may also use nitrite-based products, like leather cleaners or room deodorizers, because they believe the chemicals enhance sexual pleasure.
In addition to triggering the high, inhalants also deliver toxic chemicals to the body. The inhalant works by displacing the air inside the lungs, a process called hypoxia. Deeply breathing the vapors delivers chemicals in doses hundreds of times greater than the maximum allowed in industrial settings.
Risks of Inhalant Use
The risks include loss of coordination and inhibition as well as dangerous hallucinations and delusions. Life-threatening risks include suffocation due to the displacement of oxygen in the lungs, to heart failure from the loss of proper heart rhythm. Inhalants have also been linked to liver and kidney damage.
Brain cells are especially vulnerable to the abuse, which is why inhalants have such a profound impact on functions like memory, learning new things, and even carrying on a conversation. Inhalant use may cause permanent brain damage and death—these can happen any time a person huffs, even the first time. Users face the risk of an overdose every time they abuse the substance, making drug rehab that much more critical.
Signs of Inhalant Abuse in Adults
- Chemical odors on breath or clothing
- Hidden containers of inhalant products
- Slurred speech
- Fatigue
- Weight loss
- Hostility
- Paranoia
- Poor concentration
- Confusion
- Poor hygiene
Inhalant Abuse Treatment
This is a serious problem that requires immediate and professional treatment. Because of the risk of devastating and life-threatening consequences, there is no time to wait to see if the person will stop on his or her own. Consider using a professional interventionist to get the addict into treatment as soon as possible.
Not every drug rehab treatment center has the resources to treat inhalant abuse, so it may take several tries to find a qualified facility. To be effective, treatment must be within an inpatient setting. Detoxification is necessary, and, because the chemicals are so pervasive, that process will take several weeks. Withdrawal symptoms are common and may include hallucinations, nervousness, muscle pain, psychosis, insomnia, seizures and aggression. A medical staff will monitor the addict and provide medications to relieve symptoms and address complications.
Long-term success requires a detailed treatment strategy that addresses the addict’s entire well-being: physical, emotional and intellectual. After detox, addiction specialists will assess the addict for cognitive and physical damage caused by the inhalant. This testing provides a foundation for building a rehab plan that address all of his or her needs.
One of the challenges in treating this type of substance abuse is its effect on cognition, or thinking ability. For example, the inability to concentrate may require shorter individual treatment sessions, sometimes as brief as 15 or 20 minutes, especially at the onset of drug rehab treatment. Sessions may also be informal to accommodate an addict’s reduced ability to think and reason.
Intensive aftercare will be crucial for long-term recovery. An addict may require a sober living facility where he or she can start to live a normal life without the stresses and pressures that spur relapse. Recovery may also require career counseling and life skills training. Addicts with lasting physical side effects may need therapy to improve hand-eye coordination and other skills.
It’s likely that living accommodations will need to be made after inpatient or sober living concludes. For instance, it might be necessary to eliminate inhalable substances from work or living areas. If the recovering addict lives with others, like family or roommates, they’ll need to be aware of the problem so they can avoid inadvertently tempting the addict by, for example, keeping computer cleaning sprays in the home.
Many inhalants are highly addictive, so it’s unlikely that abusers can “will” themselves into a sober life. Recovery from inhalant abuse will not be easy. It will require medically monitored detox, inpatient treatment and long-term aftercare. The alternative, however, is devastating. Left untreated, inhalant abuse can cause serious, lasting health consequences. In some cases, it leads to permanent brain damage or death.
If someone you love is abusing inhalants, talk to them about getting treatment now–before it’s too late. A drug rehab center experienced in treating this type of substance abuse will have the resources needed to help your loved one overcome this potentially devastating addiction.
15 Apr 2013
Cocaine Use Leads to Enlarged Heart
Enlarged heart is a term that doctors use to describe a heart muscle that grows beyond its expected size, either on the whole or in part. Some forms of heart enlargement, such as those frequently found in habitual exercisers, can support improved cardiac health. However, other forms of heart enlargement make the heart increasingly dysfunctional and set the stage for life-threatening problems such as a heart attack and cardiac arrest. Cocaine use can lead to a form of heart enlargement that seriously increases risks for cardiac arrest and sudden, unpredictable death.
Background
The muscle content of the heart, called the myocardium or myocardial tissue, gives the organ the power it needs to contract and pump blood. The primary pumping chamber—known as the left ventricle—forms the lower left segment of the heart, while the secondary pumping chamber, known as the right ventricle, forms the lower right segment of the organ. The left ventricle moves oxygen-rich blood to the body’s arteries; the right ventricle moves oxygen-depleted blood to the lungs, where new supplies of oxygen enter the bloodstream. The upper left chamber of the heart—known as the left atrium—carries oxygen-rich blood to the heart from the lungs, while the upper right chamber, known as the right atrium, carries oxygen-depleted blood to the heart from the rest of the body.
Enlarged Heart Basics
The medical term for heart enlargement is cardiac hypertrophy. This phenomenon occurs when the muscular walls of the heart (i.e., the myocardium) grow unusually thick. When unusual thickness appears in either of the ventricles, the affected individual has a condition called ventricular hypertrophy; when unusual thickness appears in either of the atria (plural of atrium), the affected individual has a condition called atrial hypertrophy. As noted previously, some forms of hypertrophy can make the heart work better. For instance, athletes and regular exercisers can develop a form of ventricular hypertrophy that makes it easier for the heart to pump blood to the lungs or other parts of the body. However, as also noted previously, some forms of hypertrophy reduce the heart’s effectiveness. This typically occurs when enlargement scars and stiffens the walls of the ventricles, and thereby decreases their ability to contract and pump blood.
Damaging forms of heart enlargement are known collectively as pathological cardiac hypertrophy. Apart from cocaine use, potential underlying causes of damaging enlargement include chronic high blood pressure, a heart attack, disease in any of the valves that sit between the heart’s chambers, and heart failure. Typically, unhealthy heart enlargement develops gradually over time; however, in certain circumstances, it can also develop relatively rapidly. In many cases, dangerous cardiac hypertrophy produces no symptoms until its effects are relatively advanced. For this reason, people with the condition can die suddenly from a heart attack or from an abrupt stoppage of heart.
The Role of Cocaine
Cocaine use causes heart enlargement through a unique series of health changes, according to the results of a study published in 2006 in the Journal of Cardiovascular Pharmacology. First, the presence of the drug in the bloodstream activates a specialized type of protein (enzyme) called CaMK; in turn, activation of this enzyme encourages an abnormal buildup of the mineral calcium in the heart’s tissues. When calcium builds up in the heart, it promotes the accumulation of other proteins that normally only appear in the hearts of developing fetuses. When they first appear, these immature proteins increase the size of individual cells inside the myocardium. Eventually, enlargement spreads to larger areas of tissue and triggers the onset of cardiac hypertrophy. Typically, this process occurs in the heart’s primary pumping chamber, the left ventricle.
People who habitually use cocaine can develop degrees of hypertrophy that enlarge their left ventricles by up to 70 percent, the authors of a study published in 2003 in the Journal of Cardiovascular Pharmacology and Therapeutics report. The amount of enlargement associated with long-term cocaine use can weaken the left ventricle to the point where this chamber can no longer meet the strict timing requirements necessary to coordinate heart activity and efficiently pump blood. In turn, lack of proper heart beat timing can lead to serious forms of a condition called a heartbeat irregularity, or arrhythmia.
The degree of arrhythmia associated with long-term cocaine use can lead to unsustainable changes in heart rhythm and the unpredictable, frequently fatal appearance of cardiac arrest. Unlike people with chronic heart disease, cocaine users can easily develop enlargement-related cardiac arrest without developing symptoms—such as high blood pressure or an increase in resting heart rate—that cue doctors to the possible presence of dangerous changes in normal heart function. According to the authors of the study published in 2006 in the Journal of Cardiovascular Pharmacology, as many as half of all habitual cocaine users with normal blood pressure may have some degree of heart enlargement.
Sizzurp is a common slang term for a recreational drug concoction based on promethazine/codeine syrup, a prescription medication used to control coughs and other symptoms related to allergies, colds, and certain additional upper respiratory ailments. In early 2013, this concoction gained new prominence in the media through its connection with a popular hip-hop performer named Lil’ Wayne, who suffered a series of seizures believed to be directly related to his sizzurp intake. In addition to seizures, use of sizzurp can potentially trigger the onset of neuroleptic malignant syndrome, a sometimes fatal condition linked to the intake of the medication promethazine.
 Sizzurp Basics
Sizzurp Basics
Sizzurp qualifies as a recreational drug of abuse because it contains codeine, an opioid narcotic that can produce addiction through repeated use by altering the way the brain creates and uses dopamine, a neurotransmitting chemical responsible for triggering a profound form of pleasure called euphoria. Although specific formulas for making the concoction vary, most batches of sizzurp are based on promethazine/codeine syrup, which contains roughly 6 parts of promethazine for every 10 parts of codeine; the syrup also contains a small amount of alcohol. Other common ingredients in a sizzurp mixture include clear sodas, clear types of alcohol, and melted candies or some other additional source of sugar. People who drink sizzurp often display a characteristic loss of body balance and associated walking difficulties. Apart from these balance changes and euphoria, effects of the concoction typically include a sleep-promoting state called sedation and impairment of the brain’s higher mental faculties.
Promethazine Basics
Promethazine (known more formally as promethazine hydrochloride) is an antihistamine; this means that it counters the effects of histamine, a naturally occurring substance in the body that triggers sneezing, a runny nose, and other symptoms that commonly appear in people who have certain types of allergies. Chemically speaking, promethazine is also classified as a phenothiazine and a neuroleptic. The term phenothiazine describes a variety of substances that act as antihistamines or antipsychotic drugs when they enter the human body. Doctors and scientists sometimes use neuroleptic as an alternative term for any antipsychotic drug.
Neuroleptic Malignant Syndrome
Neuroleptic malignant syndrome (NMS) is a rare but very serious medical condition that occurs when the effects of promethazine or some other neuroleptic or antipsychotic medication make certain unwanted changes in the normal function of the central nervous system (brain and spinal cord). Although no one knows for sure what causes these changes, one likely candidate appears to be alteration of the brain’s ability to properly process dopamine, the same neurotransmitting chemical linked to the onset of codeine addiction (as well as addiction to almost all other well-known substances of abuse). This connection to NMS is possible because dopamine has other important functions inside the brain, including assisting in the regulation of normal body temperature and regulation of the basic ability to control muscle movement. When dopamine levels change, they can produce profound alterations in these functions.
The National Institute of Neurological Disorders and Stroke lists potential symptoms of NMS that include abnormal muscle rigidity, dangerously elevated body temperature (known medically as hyperthermia or hyperpyrexia), and reduced or altered mental awareness. NMS can also produce significant changes in the normal function of the autonomic nervous system, an involuntary nerve network that helps control ongoing function in the body’s vital organs. Specific changes in this system associated with the effects of NMS can include a rapid heartbeat (tachycardia), unusually rapid breathing, an unstable pulse, unstable blood pressure, abnormally high sweat output, and a form of heartbeat irregularity known variously as an arrhythmia or a dysrhythmia. Ultimately, the effects of neuroleptic malignant syndrome can escalate to a point where they become deadly.
Considerations in Sizzurp Users
Normally, doctors control the risks for neuroleptic malignant syndrome in promethazine/codeine syrup users by limiting the prescribed intake of the medication and screening their patients for the presence of underlying factors that can contribute to the development of the disorder. However, since sizzurp users take promethazine/codeine outside of the context of medical treatment, they don’t receive the benefits of a doctor’s guidance. This makes it likely that very few people who use sizzurp have ever heard of NMS, or have any understanding of the risks they’re taking by using promethazine without a prescription or a physician’s input. It also means that affected individuals may fail to recognize the initial effects of NMS, and therefore may fail to seek help for their condition until serious or severe health complications arise. Since sizzurp use is fairly new from a medical research standpoint, no one really knows how many people are at risk for the unexpected onset of NMS.
04 Apr 2013
Long Term Effects of OxyContin on the Brain
 Most drugs of abuse ultimately have an impact on the brain. The levels of the different neurotransmitters (the brain’s chemical messengers) are carefully balanced, so the brain can apply a reward chemical when a reward is in order and a painkiller when one is required. Drugs of abuse tend to subvert these normal processes, often releasing an excessive amount of the brain’s reward chemical. Finding out about the specific risks for one of the most commonly abused prescription drugs, OxyContin, helps you understand how addiction develops and the long-term risks of the drug.
Most drugs of abuse ultimately have an impact on the brain. The levels of the different neurotransmitters (the brain’s chemical messengers) are carefully balanced, so the brain can apply a reward chemical when a reward is in order and a painkiller when one is required. Drugs of abuse tend to subvert these normal processes, often releasing an excessive amount of the brain’s reward chemical. Finding out about the specific risks for one of the most commonly abused prescription drugs, OxyContin, helps you understand how addiction develops and the long-term risks of the drug.
What is OxyContin?
The simplest way to understand OxyContin is as an opioid drug like heroin or opium. It is derived from the same source, and has the same basic effects as these illicit substances. Opioids are widely used in medicine because they are among the most efficient pain relievers. Many people come into contact with drugs such as Vicodin, Percocet and OxyContin through legitimate means. The main defining feature of OxyContin is that it has a time-release formula, the effects lasting for about 12 hours. Percocet releases all of the substance at once and lasts only about five hours.
What are the Effects of OxyContin?
OxyContin works through its interaction with the opiate receptors in the brain. By binding to these receptors, the drug reduces feelings of pain and triggers the release of dopamine, the most important neurotransmitter in the brain’s reward system. This creates a mixture of euphoria and pain relief, bringing about a relaxed and contented mood in the user. It also depresses the central nervous system, which is responsible for many critical processes within the body, including heart rate, digestion, pain messages and breathing. Although the time-release formula makes it more difficult to achieve the euphoric high most users are looking for, many chew the drug or even inject it for a bigger rush. They will also take more than is suggested by their doctor to increase the effect.
 The Long-Term Effects of OxyContin on the Brain
The Long-Term Effects of OxyContin on the Brain
Addiction is the most evident effect of long-term OxyContin abuse on the brain. The brain is initially overwhelmed when the drug signals the extended release of dopamine, unable to continue its normal functioning because of the intense chemical injection. To account for this, as the drug is taken more regularly, the brain adjusts its natural processes so it isn’t overwhelmed anymore. By reducing the number of opiate receptors and producing less dopamine naturally, the brain effectively dampens the effect OxyContin has. This means that the user has to take more of the drug to achieve the same effect, and that without the drug, he or she will have a deficit in some neurotransmitters.
This effect creates addiction, because the brain has essentially rewired itself to account for the continued presence of the particular substance. Without it, the individual experiences a wide range of unpleasant side effects, known as withdrawal. The longer the individual takes the drug and the more that is consumed, the more the brain adapts and the individual becomes addicted. Although using OxyContin more than prescribed commonly leads to addiction, it can also develop from the suggested course of medication.
Many of the long-term effects of the drug come to the forefront during this withdrawal period. Withdrawal usually creates the opposite effect of the drug, so if a woman goes without OxyContin for the first time after months of abuse, she will experience severe pain, depression and flu-like symptoms such as loss of appetite, runny nose and sneezing. Irritability and mood swings are also common. Because of these effects, the cravings for another dose of the drug can be intense.
One of the main risks of any opioid drug is respiratory depression (or slowed breathing). This is because the drugs depress the central nervous system, which is responsible for breathing. The risk of this is greater in long-term users, those who take more of the drug than prescribed, and anybody who combines it with alcohol.
Finally, there is a risk of severe psychological disturbances in people who abuse OxyContin. In long-term users, hallucinations, delusions, and delirium have all been reported, in addition to mood swings and panic attacks. This doesn’t occur in all cases, but is often worse during withdrawal, when many users feel confused or disoriented. Memory issues or even amnesia can develop in long-term abusers.
Need for Psychological Support
Addiction is the major long-term effect of OxyContin use because it drives the individual to keep abusing the drug and thereby makes all of the other potential consequences more likely. Being able to recognize the signs of addiction is extremely useful, but the best way to minimize your risk is to take the drug as advised by your doctor. If addiction does occur, psychological support can help you overcome your issues and therefore reduce the risk of other ill-effects.
The blood-brain barrier (BBB) is a network of tiny blood vessels (capillaries) that separates the interior of the central nervous system (brain and spinal cord) from the rest of the body’s circulatory system. This separation is required to help the brain maintain a stable internal environment and function properly; it also helps protect the brain from infectious microorganisms. Cocaine and methamphetamine can significantly damage normal function in the blood-brain barrier; in turn, this damage can open up the brain to infection and other processes that can produce severe or life-threatening changes in brain health.
Blood-Brain Barrier Basics
Capillaries are the body’s smallest blood vessels. They sit at the junction between the arteries—which carry oxygen-bearing blood to various organs and tissues—and the veins, which carry oxygen-depleted blood and carbon dioxide waste from the organs and tissues to the heart (on the way to their eventual destination point in the lungs). It’s inside the capillaries where exchange of the oxygen and carbon dioxide content in the blood occurs.
In every location except the blood-brain barrier, the capillaries have relatively large openings in their walls that allow large and small molecules to move in and out of the bloodstream. This level of access means that any required substance produced in most of the body can easily travel through the bloodstream and get where it needs to go. However, it also means that conditions in the tissues fed by the capillaries can change rapidly and relatively chaotically as different molecules move in and out of circulation.
The central nervous system in general (and the brain in particular) can’t handle the sorts of fluctuations that occur when all molecules can flow easily through the capillary walls. In fact, these fluctuations would destabilize the brain to the point where it wouldn’t be able to perform its function as the body’s command and control center. In addition, if any molecule could easily enter the central nervous system, then infectious microorganisms could get to the brain and wreak all sorts of havoc on the organ’s structures and activities. In order to help prevent these possibilities, the capillaries in the BBB are very tightly constructed and lack the large openings found in other capillaries. In addition, supporting cells (called astrocytes) sit in the barrier outside the capillary walls and further block any influx of unwanted molecules and microorganisms.
The Effects of Cocaine and Methamphetamine
For a number of reasons having to do with how cell walls are constructed, molecules that dissolve easily in the presence of fat can pass directly through the capillary walls in the blood-brain barrier. Among the molecules that can access the central nervous system in this way are cocaine and methamphetamine. Once inside the central nervous system, these drugs produce mind alteration and a variety of other effects by altering the normal levels of certain neurotransmitting chemicals—such as dopamine, norepinephrine and serotonin—that support proper brain function by passing on required messages between millions of nervous system cells called neurons.
 One of the consequences of neurotransmitter alteration by cocaine and methamphetamine is a significant increase in the amount of heat retained inside the brain and body. If heat levels get too high, they can trigger a condition called hyperthermia, which literally means “overheat.” In turn, hyperthermia can produce serious damage in the capillary walls inside the blood-brain barrier and lead to the formation of significant gaps that give access to dangerous molecules not usually allowed into the central nervous system’s restricted environment.
One of the consequences of neurotransmitter alteration by cocaine and methamphetamine is a significant increase in the amount of heat retained inside the brain and body. If heat levels get too high, they can trigger a condition called hyperthermia, which literally means “overheat.” In turn, hyperthermia can produce serious damage in the capillary walls inside the blood-brain barrier and lead to the formation of significant gaps that give access to dangerous molecules not usually allowed into the central nervous system’s restricted environment.
Apart from its role in hyperthermia, cocaine produces chemical changes in the capillary walls that lead to the formation of abnormally large points of entry through the BBB, according to a study published in 2010 in Blood, the journal of the American Society of Hematology. These chemical effects are particularly prominent in cocaine users who have HIV infections, and the authors of the study believe that the relatively rapid advancement of HIV’s brain effects in cocaine users stems from the ability of both cocaine and HIV to damage the capillary structures in the blood-brain barrier. Cocaine may also damage the BBB by increasing the flow of blood plasma to the brain, or by encouraging an excessive flow of the neurotransmitter serotonin from the body to the brain. In addition to its role in hyperthermia, methamphetamine can apparently damage the blood-brain barrier through a direct, toxic effect on the capillaries within the barrier.
Substituted amphetamines are a group of chemically related substances that possess a strong chemical resemblance to the manmade stimulant drug amphetamine. Some of these substances-including ephedrine, pseudoephedrine, and cathinone-come from plant sources and predate synthetic amphetamine by thousands of years or more. Others-including methamphetamine and MDMA (Ecstasy)-are synthetic and have only existed for anywhere from decades up to slightly more than a century. Almost all substituted amphetamines produce pleasure and stimulant effects in the central nervous system; to varying degrees, they may also produce hallucinations and increased feelings of connectedness toward others. Side effects common to most of these substances include potentially deadly toxic reactions (overdoses) and long-term risks for drug addiction.


